Mental health conditions are associated with a significant burden on individuals. Using data from a large population health survey, the present study aimed to quantify the burden of emotional disorders (depression and anxiety) on health-related quality of life (HRQoL) in the region of Catalonia (Spain) for evidence-informed policy making.
MethodsRegression models were used to estimate the impact of emotional disorders on HRQoL, controlling by socioeconomic factors and somatic health problems. The rate of emotional disorders was based on the General Health Questionnaire (GHQ-12) and quality of life scores were based on the EQ-5D.
ResultsThe impact of emotional disorders on HRQoL was equal to a reduction of 0.17 in the EQ-5D score. Translation of this individual impact to population figures yielded a total loss of 78,742 quality-adjusted life years (QALYs) for 2006. This strong impact highlights the need for global policies aiming to reduce this burden.
ConclusionThe negative relation between emotional disorders and the HRQoL of individuals was confirmed and quantified for the population of Catalonia. The use of quality of life scales such as the SF or EQ-5D, combined with data on quasi-specific health conditions provides substantial information for prioritizing and planning health programs.
Los trastornos mentales suponen una importante carga sobre los individuos. A partir de los datos de una encuesta de salud poblacional, el presente estudio cuantifica la carga que suponen los trastornos emocionales (depresión y ansiedad) sobre la calidad de vida relacionada con la salud (CVRS) en Cataluña (España) para una política basada en evidencia informada.
MétodoSe utilizó un modelo de regresión para evaluar el impacto de los trastornos depresivos y de ansiedad sobre la CVRS, controlando por factores socioeconómicos y por otras condiciones de salud. La prevalencia de los trastornos mentales se basó en el Cuestionario de Salud General (GHQ-12), y para obtener la valoración de la calidad de vida se empleó el cuestionario EQ-5D.
ResultadosEl impacto de los trastornos emocionales en la CVRS equivale a una reducción de 0,17 en la puntuación del EQ-5D. Este impacto individual, cuando se traslada a cifras poblacionales, equivale a una pérdida de 78.742 años de vida ajustados por calidad para el año 2006. Esta importante cifra señala la necesidad de políticas globales que tengan como objetivo la reducción de esta carga.
ConclusiónEste estudio confirma y cuantifica para la población de Cataluña la relación negativa entre los trastornos emocionales y la CVRS. El empleo de escalas de calidad de vida, como el SF y el EQ-5D, combinadas con información sobre condiciones de salud, proporciona datos relevantes para la priorización y la planificación de programas sanitarios.
The epidemiological transition from acute to chronic illness has stimulated a change in outcome measurement in healthcare. Mortality figures alone are inadequate to accurately reflect the burden of distinct health conditions. Consequently, outcome measures based on functioning, disability and health-related quality of life (HRQoL) have been proposed.1,2
Mental health conditions are associated with a significant burden on individuals, reducing their quality of life and impairing their capacity to fulfil their individual potential. Consequently, the burden of these conditions on individuals and populations is better assessed with disability and quality of life measures, rather than with mortality data alone. The World Health Organization (WHO) assessed the burden of disease of several health conditions based on epidemiological data of disease prevalence and on estimates of the impact of distinct conditions on individuals’ health2 and found that depression was the third greatest cause of health disability worldwide and the second in the developed world.3 Projections suggest that depression will be the main cause of health disability (6.2% of the global burden of disease) in 2030, more than that associated with ischemic heart diseases or road traffic accidents.
Another approach to estimate the burden of mental health conditions relies on analyzing individual data to estimate the impact of these disorders on HRQoL.4 Individual data allows the marginal effect of mental health conditions on HRQL to be estimated, controlling by comorbid factors and other variables that might also affect the outcome measure.
Evidence-informed care is a new approach to health policy making that incorporates various sources of local information apart from traditional evidence-based research.5,6 Local evidence (e.g. regional information) is critical for making decisions about health policies, and periodic national and regional health surveys constitute a major tool for evidence-informed policy making. However the interpretation of data on psychiatric disorders and emotional distress in general health surveys poses additional challenges to planning and priority setting, mainly due to the inherent nosological complexity of these disorders, especially that of the construct of emotional disorders (depression/anxiety)7; interpretation is also hampered by problems of the reliability and validity of brief assessment measures used in these surveys.
To generate an informed evidence base for planning and priority setting, in 2008 the Catalan Department of Health commissioned a series of related studies on the burden and costs of depression in Catalonia (COSTDEP8). The cost of illness analysis confirmed the major impact of depression on both the health sector and employment.9 This analysis also demonstrated the difficulties of disaggregating information on anxiety and depression outside specialized care, due to the proportion of mixed anxiety and depression in primary care as well as in disability pension records.
The present study aimed to quantify the burden of emotional distress (depression and anxiety) in the region of Catalonia, one of the seventeen autonomous regions in Spain, using a large population health survey. A further aim was to assess the utility of this database for mental health planning and priority setting.
MethodsThis study formed part of the COSTDEP project.8 The organizations involved in this project included the Catalan Department of Health, the London School of Economics and Political Science, and the research association PSICOST. An expert panel, which included researchers, clinicians, providers, decision makers and managers of health databases relevant for depression in Catalonia, also participated.9 The expert panel consisted of two groups; the first group (group A) was formed by nine experts in the distinct topics related to the study (epidemiology, use of services, resources management, costs) while the second group (group B) was composed of nine officers and health decision makers from various units of the Catalan Department of Health and other official entities, as well as the managers of databases or related studies and programs (names are provided in the acknowledgements section). Group A held two meetings with a mean length of 3hours while group B undertook three work meetings.
DataThe data source for all of the analyses was the Catalonian Health Survey of 200610 (Encuesta de Salud de Catalunya 2006, ESCA), a cross-sectional survey that collected information about morbidity, health status, health-related behaviors, use of health care services, and sociodemographic data from a representative sample of the non-institutionalized population of Catalonia. In total, 18,126 persons (15,926 aged 15 years or over, and 2,200 under 15 years) were randomly selected using a multiple-stage process and were interviewed at home by trained interviewers. All interviews were conducted between December 2005 and July 2006.10 For this analysis, only data from individuals aged 15 years or over were selected.
The ESCA 2006 provides information on the mental health status of individuals, based on the 12-item version of the General Health Questionnaire (GHQ-12). This instrument is a screening questionnaire designed for use in consulting settings and aimed at detecting individuals with a diagnosable psychiatric disorder.11 The GHQ-12 can be used to provide an indication of the proportion of ‘emotional distress’12 or as a screening instrument in epidemiological studies of mental disorders.13 The validated cut-off point for the Spanish version of the GHQ-12 is equal to a score of 2/3,14 implying that individuals with a score of 3 and higher are considered likely to have a psychiatric disorder. Nevertheless, this cut-off point is usually used in double-phase screening studies. In this analysis, to determine the optimal cut-off point to establish that an individual had an emotional disorder (depressive and/or anxiety disorder),7 a consultation round was made with the main experts in the use of GHQ in Spain. Finally a conservative approach was adopted to reduce the possible number of false positive results and this option was agreed by the COSTDEP expert panel. Therefore, for this analysis, individuals with a score of 4 or higher were considered to probably have an emotional disorder.
HRQoL is that part of an individual's quality of life that can potentially be influenced by health and healthcare. In the ESCA 2006, HRQoL was measured with the widely used EQ-5D.15 This tool measures health status across five dimensions (mobility, self-care, usual activities, pain or discomfort and anxiety or depression) and each dimension has three grades of severity corresponding to no, moderate or extreme problems; consequently, the EQ-5D can capture 243 different health states. Each of these health states is assigned a utility score elicited from the general population's preferences, with a value of 1 corresponding to perfect health and a value of 0 to death; health states can be valued as being worse than death and are assigned negative scores. The utility scores used have been validated for the Spanish population, obtained through the time trade-off method.16 Usually, these health utilities are combined with the duration of the health states to obtain quality adjusted life years (QALYs).1 However, the ESCA 2006 is a cross-sectional survey and therefore, in this study, when QALYs were calculated, their values only reflected the impact of poor health on quality of life, rather than on the duration of life.
The socioeconomic factors included in the analysis were age, sex, living arrangements (living alone, with a partner or with other people) and educational attainment (primary education not completed, primary education, secondary education and higher education). The variable of social class, based mainly on last professional occupation,17 was also included as a proxy of individuals’ incomes. ESCA 2006 contains information on somatic health problems, which was used in the analysis. Participants were asked (separately for each condition) whether they were suffering or ever had suffered from a list of chronic health conditions including heart and pulmonary diseases, cancer, diabetes and back pain, among others.
AnalysesThe impact of emotional disorders (depression and anxiety) on HRQoL was analyzed through a regression model, with the socioeconomic factors and chronic somatic conditions as covariates. The dependent variable, the HRQoL measure, has a ceiling effect, with 57% of the sample scoring full health on the EQ-5D in the ESCA sample. Therefore, a multiple regression model for censored data, the Tobit model,18 was used. The marginal effect of the variable of depressive and anxiety disorders for the unconditional expected value of the HRQoL score, evaluated at the means of the explanatory variables,19 was interpreted as the change in HRQoL score associated with the mental health condition. The loss of HRQoL, or the burden due to this condition for the Catalan population, was then estimated by multiplying this individual effect of the mental health conditions on HRQoL by the prevalence of the conditions.4 This figure, measured in QALYs, is the impact of depressive and anxiety disorders on the Catalan population's HRQoL for 2006, without considering the effect of these disorders on mortality.
Sensitivity analysesThe same method was employed for two other approaches to estimate the rate of emotional disorders. First, a score of 3 or higher was used as the cut-off value in the GHQ-12 (the validated cut-off point for the Spanish version of the instrument) to categorize individuals as having emotional disorders. Second, the rate of these disorders was based on the individuals who reported that they were suffering or had suffered from emotional disorders in response to the survey question on chronic health conditions.
ESCA weights were used to ensure that the results of the analyses would be representative of the Catalan population. Analyses were performed using SPSS version 15 for Windows (SPSS Inc., Chicago, USA) and Stata version 10 for Windows (Stata Corp., College Station).
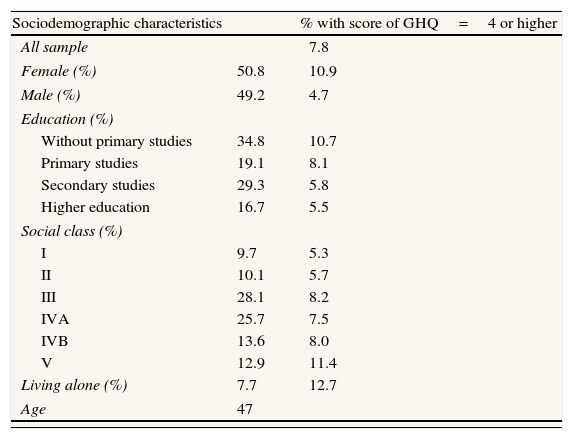
ResultsThe socioeconomic characteristics of the (weighted) sample are shown in Table 1, along with the rate of emotional disorders (GHQ=4 or higher) by sociodemographic categories.
Sociodemographic characteristics of the sample.
| Sociodemographic characteristics | % with score of GHQ=4 or higher | |
| All sample | 7.8 | |
| Female (%) | 50.8 | 10.9 |
| Male (%) | 49.2 | 4.7 |
| Education (%) | ||
| Without primary studies | 34.8 | 10.7 |
| Primary studies | 19.1 | 8.1 |
| Secondary studies | 29.3 | 5.8 |
| Higher education | 16.7 | 5.5 |
| Social class (%) | ||
| I | 9.7 | 5.3 |
| II | 10.1 | 5.7 |
| III | 28.1 | 8.2 |
| IVA | 25.7 | 7.5 |
| IVB | 13.6 | 8.0 |
| V | 12.9 | 11.4 |
| Living alone (%) | 7.7 | 12.7 |
| Age | 47 | |
| EQ-5D | All sample | GHQ=4 or higher | GHQ=3 or lower | Difference |
| Mean score | 0.86 | 0.58 | 0.90 | 0.32a |
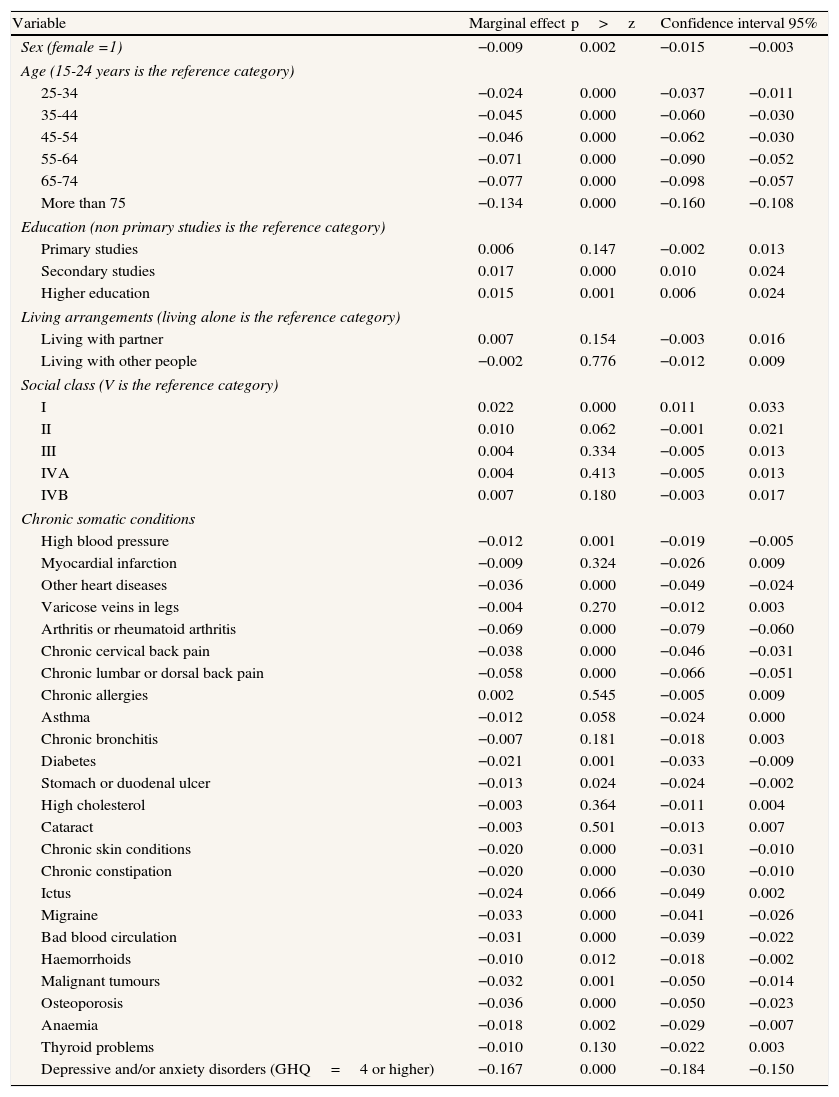
The whole sample rate of these disorders was 7.8% with 4.7% among men and 10.9% among women. Higher rate figures were found among persons with lower educational attainment and those living alone. The mean EQ-5D score was statistically significantly lower in individuals with a GHQ score of 4 or higher. The regression model estimated the marginal effect of the variables for the unconditional expected value of the HRQoL score, evaluated at the means of the explanatory variables. These values and their 95% confidence intervals are shown in Table 2.
Multiple regression model (Tobit); impact on HRQL of emotional disorders (depression and anxiety).
| Variable | Marginal effect | p>z | Confidence interval 95% | |
| Sex (female =1) | −0.009 | 0.002 | −0.015 | −0.003 |
| Age (15-24 years is the reference category) | ||||
| 25-34 | −0.024 | 0.000 | −0.037 | −0.011 |
| 35-44 | −0.045 | 0.000 | −0.060 | −0.030 |
| 45-54 | −0.046 | 0.000 | −0.062 | −0.030 |
| 55-64 | −0.071 | 0.000 | −0.090 | −0.052 |
| 65-74 | −0.077 | 0.000 | −0.098 | −0.057 |
| More than 75 | −0.134 | 0.000 | −0.160 | −0.108 |
| Education (non primary studies is the reference category) | ||||
| Primary studies | 0.006 | 0.147 | −0.002 | 0.013 |
| Secondary studies | 0.017 | 0.000 | 0.010 | 0.024 |
| Higher education | 0.015 | 0.001 | 0.006 | 0.024 |
| Living arrangements (living alone is the reference category) | ||||
| Living with partner | 0.007 | 0.154 | −0.003 | 0.016 |
| Living with other people | −0.002 | 0.776 | −0.012 | 0.009 |
| Social class (V is the reference category) | ||||
| I | 0.022 | 0.000 | 0.011 | 0.033 |
| II | 0.010 | 0.062 | −0.001 | 0.021 |
| III | 0.004 | 0.334 | −0.005 | 0.013 |
| IVA | 0.004 | 0.413 | −0.005 | 0.013 |
| IVB | 0.007 | 0.180 | −0.003 | 0.017 |
| Chronic somatic conditions | ||||
| High blood pressure | −0.012 | 0.001 | −0.019 | −0.005 |
| Myocardial infarction | −0.009 | 0.324 | −0.026 | 0.009 |
| Other heart diseases | −0.036 | 0.000 | −0.049 | −0.024 |
| Varicose veins in legs | −0.004 | 0.270 | −0.012 | 0.003 |
| Arthritis or rheumatoid arthritis | −0.069 | 0.000 | −0.079 | −0.060 |
| Chronic cervical back pain | −0.038 | 0.000 | −0.046 | −0.031 |
| Chronic lumbar or dorsal back pain | −0.058 | 0.000 | −0.066 | −0.051 |
| Chronic allergies | 0.002 | 0.545 | −0.005 | 0.009 |
| Asthma | −0.012 | 0.058 | −0.024 | 0.000 |
| Chronic bronchitis | −0.007 | 0.181 | −0.018 | 0.003 |
| Diabetes | −0.021 | 0.001 | −0.033 | −0.009 |
| Stomach or duodenal ulcer | −0.013 | 0.024 | −0.024 | −0.002 |
| High cholesterol | −0.003 | 0.364 | −0.011 | 0.004 |
| Cataract | −0.003 | 0.501 | −0.013 | 0.007 |
| Chronic skin conditions | −0.020 | 0.000 | −0.031 | −0.010 |
| Chronic constipation | −0.020 | 0.000 | −0.030 | −0.010 |
| Ictus | −0.024 | 0.066 | −0.049 | 0.002 |
| Migraine | −0.033 | 0.000 | −0.041 | −0.026 |
| Bad blood circulation | −0.031 | 0.000 | −0.039 | −0.022 |
| Haemorrhoids | −0.010 | 0.012 | −0.018 | −0.002 |
| Malignant tumours | −0.032 | 0.001 | −0.050 | −0.014 |
| Osteoporosis | −0.036 | 0.000 | −0.050 | −0.023 |
| Anaemia | −0.018 | 0.002 | −0.029 | −0.007 |
| Thyroid problems | −0.010 | 0.130 | −0.022 | 0.003 |
| Depressive and/or anxiety disorders (GHQ=4 or higher) | −0.167 | 0.000 | −0.184 | −0.150 |
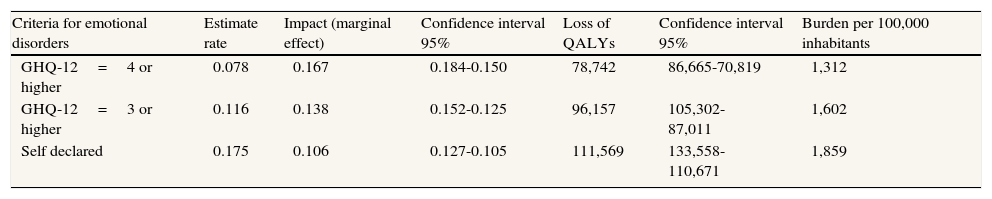
After controlling for socioeconomic factors and chronic somatic disorders, the regression results show that the impact of depressive and anxiety disorders on HRQoL was equal to a reduction of 0.17 in the EQ-5D score, the factor with by far the highest impact among those comprising the model, including all other health conditions reported by survey respondents. The translation of this individual impact to population figures gave a total loss for 2006 of 78,742 QALYs due to depressive and anxiety disorders (without considering mortality), among the non-institutionalized Catalan adult population. This loss equated to a burden of 1,312 QALYs per 100,000 inhabitants (Table 3).
Annual losses of QALYs associated to emotional disorders (depression and anxiety).
| Criteria for emotional disorders | Estimate rate | Impact (marginal effect) | Confidence interval 95% | Loss of QALYs | Confidence interval 95% | Burden per 100,000 inhabitants |
| GHQ-12=4 or higher | 0.078 | 0.167 | 0.184-0.150 | 78,742 | 86,665-70,819 | 1,312 |
| GHQ-12=3 or higher | 0.116 | 0.138 | 0.152-0.125 | 96,157 | 105,302-87,011 | 1,602 |
| Self declared | 0.175 | 0.106 | 0.127-0.105 | 111,569 | 133,558-110,671 | 1,859 |
The rate of emotional disorders among the Catalan population, when evaluated using the GHQ-12 cut-off point of a score of 3 or higher, was 11.6%, with values of 7.6% for men and 15.5% for women. The other alternative, using self-reported data on suffering or having suffered from emotional disorders, resulted in rate figures for the whole sample of 17.5% overall (11% for men and 23.8% for women). These rate figures were higher than those found in the main analysis and the individual impact of these disorders on health utility was lower. Nevertheless, total population losses of QALYs were higher as a result of larger proportions of individuals suffering from emotional disorders (Table 3).
DiscussionPrevious studies20,21 have shown that depressive and anxiety disorders have a strong impact on HRQoL. This study confirms these findings from a health policy perspective and stresses that the associated burden reached substantial values even when the impact on mortality was not measured. The sensitivity analyses generated distinct results but do not alter the broad message that these disorders substantially impair quality of life.
The relevance of these findings on the effect of these mental health conditions on individuals’ lives is reinforced by the fact that the analysis controls for the influence of sociodemographic variables and chronic health conditions on HRQoL. The representativeness and soundness of the findings are supported by the data employed: the individual characteristics of almost 16,000 individuals, providing a representative sample of the population of Catalonia.
These results highlight the need for global policies, not just from the mental health field, aiming to reduce this burden. The Mental Health Plan of Catalonia in 200622 recognized this need and interventions with this objective (e.g. mental health promotion programs in schools, suicide prevention programs, and improvement of early detection and treatment of depression in primary care) are being implemented.
The negative relationship found in this study between HRQoL and depressive and anxiety disorders has previously been shown using large health survey data.23 A specific relationship has also been found between GHQ-12 scores and HRQoL measured with the EQ-5D in a Spanish population.24 Studies employing similar methods have found slightly higher marginal impacts of depressive and anxiety disorders on HRQoL than found in the present study.4,25 Nevertheless, in these studies, the prevalence of depression and anxiety disorders was assessed through psychiatric interviews and therefore the individuals identified as having these disorders may have had more severe disturbance than subjects in the present study. Indeed, in the other study with a general population sample4 the prevalence of the mental health conditions analyzed was lower.
The factor with the highest impact on HRQoL among those included in the model was emotional disorders. The presence of chronic lumbar or dorsal back pain implied a reduction of 0.058 in the EQ-5D score and the figure for chronic cervical pain was 0.038 compared with 0.167 for emotional disorders. However, the prevalence rate of these conditions was higher, with almost 30% of the sample reporting they suffered or had suffered from each of them (29.6% and 27.4%, respectively). This finding is reflected by figures and comparisons of population impact, with chronic lumbar or dorsal back pain implying a burden of 1,730 QALYs per 100,000 inhabitants and chronic cervical pain a burden of 1,053 compared with the result of 1,312 QALYs per 100,000 inhabitants for emotional disorders.
Comparison with similar studies highlights the main limitation of this analysis: the method of assessing individuals as having emotional disorders in the general health surveys in Spain. The GHQ-12 was initially developed to screen for general mental disorders but proved to be more effective in screening for depression and anxiety than other psychiatric disorders.13 This instrument has also proven to be a good proxy measure of emotional distress.12 Nevertheless, the GHQ-12 has become a broadly accepted measure of psychological distress/psychiatric disorders in health surveys in Europe. However, analysis of data from the GHQ-12 for policy decision making is controversial, particularly in countries where the specific predictive validity of this instrument for assessing emotional disorders has yet to be published, as is the case in Spain.
The GHQ-12 and the Mental Health Index (MHI-5 derived from the SF-36) are the main short-form scales for the assessment of general mental status in health surveys.26 The MHI-5 has been used in the Eurobarometer 58.2,27 while the GHQ-12 is also the standard measure for the assessment of mental health in national and regional health surveys in Europe23 and is included in all regional health surveys in Spain.24 The two scales have shown a high correlation.26,28 However, there are major differences in the use of the two instruments, as the GHQ-12 has proven psychometric properties that go beyond its use as a generic mental health status measure. On the one hand, the GHQ-12 has shown a three-dimensional structure in its Spanish validation: self-esteem, stress and successful coping.29 On the other hand, this instrument can be used to identify psychiatric caseness.
These findings have led to distinct strategies to analyze depression/anxiety: the GHQ-12 and HRQoL data from health surveys for policy decision making in Spain.
One strategy has been to use a series of survey questions related to depression and anxiety despite the low reliability of this method. The following questions have been considered: 1) “Have you suffered from depression or anxiety over the previous 12 months?”; 2) “Has your physician confirmed the diagnosis?”; 3) “Have you taken antidepressants prescribed by your physician over the last 2 weeks?”; and 4) “Have you taken anxiolytics prescribed by your physician over the last 2 weeks?”. Participants who gave positive answers to questions 1, 2, and 3 or to all questions were considered “depression sufferers” and those giving positive answers to questions 1, 2, and 4 were considered “anxiety sufferers”.30
Another strategy has been to use only data from HRQoL instruments such as the SF-3628 or EQ-5D16; but this option misses the additional information provided by the GHQ. A further option, previously used in the Catalan Health Survey of 1994, was to rank the order of probability of being a psychiatric case according to the GHQ-12 rating, by using a logistic regression analysis31 but, according to the officers of the Catalan Department of Health, the information obtained with this option was of limited utility for informed policy making. The combined use of the GHQ-12 and EQ5-D has previously been used in the Canary Islands and the findings enabled health-state values to be derived from GHQ-12 scores for populations in which utilities had not, or could not, be measured directly.24
Criticisms of the combined use of both measures are based on the low reliability and predictive validity of the diagnosis of depression and anxiety disorders in health surveys and the inadequate use of screening instruments in these surveys. Based on these criticisms, GHQ information provided in annual health surveys in Spain, both nationally and regionally, should not be used to generate information relevant for policy making. These criticisms overlook the fact that levels of accuracy are related to the aim of the analyses. Obviously, if the analysis is intended to select among treatment alternatives, high accuracy and focus on specific childhood categories (e.g. major depression, generalized anxiety disorder) are required. However when the analysis is related to general priority setting32 broader parent categories may be more useful (e.g. emotional disorders), and lower levels of accuracy are admissible insofar as the same measures and scales are used to compare distinct conditions and/or population groups.
In this scenario, estimation of the annual ratio of emotional disorders as a proxy measure of the combined prevalence of anxiety and depressive disorders may be highly relevant when combined with EQ-5 data to estimate the relative burden of this grouping of psychiatric disorders in relation to groupings of other health conditions. The predictive validity and ROC curves of the GHQ-12 have recently been produced for psychiatric screening in Spain.33 In this study, the 3/4 cut-off score was selected instead of the cut-off for double phase prevalence studies in Spain (2/3). This decision was made in agreement with the experts who standardized the Spanish GHQ scales in Spain,14 as the cut-off point is not a fixed value and can be adjusted depending on the aim of the study, in the present case to reduce false-positives and to increase specificity in order to provide a conservative estimate of the comparative burden of emotional disorders in Catalonia. This approach may improve the combined analysis of results from short-form scales and QoL scales in health survey studies.
The use of quality of life scales such as the SF or EQ-5D,34 combined with data on quasi-specific health conditions, and calculation of global indexes such as QALYs provides substantial information to rank health priorities and either support or dismiss health policy programs in highly complex areas such as mental health. This regional and/or local information is critical to complement global information to fix priority setting and support informed health policy.6
A more refined way of evaluating the rate of physical health conditions would be to improve the analysis. The self-reported measures used include past and present health problems, a method that most probably has lower validity than a physical examination by a health professional. Additionally, the analysis was based on a survey that did not collect information on institutionalized individuals or on the impact of the conditions analyzed on mortality. Finally, cross-sectional data were used and therefore the method employed relies on the assumption that the results are representative for the 12-month period.
In conclusion, the present study used data from more than 15,000 individuals and highlights the substantial impact of emotional disorders on the lives of affected individuals; this negative association was confirmed and quantified for the population of Catalonia. Health policy makers should consider this impact when developing strategies to reduce the burden of health conditions on individuals and society.
What is known about this topic?Mental health conditions are associated with a significant burden on individuals, reducing their quality of life and impairing their capacity to fulfil their individual potential. The quantification of this burden for the population of Catalonia using a large population health survey can be used for evidence-informed policy making.
What does the study add to the literature?The present study confirms and quantifies the substantial negative impact of emotional disorders on the lives of affected individuals, using data from Catalonia. The results highlight the need for global policies, not just from the mental health field, aiming to reduce this burden.
Author's contributionsR. Sabes-Figuera performed the data analysis, participated in the interpretation of the data and drafted the manuscript. M. Knapp, M. Bendeck and L. Salvador-Carulla reviewed the analysis, participated in the interpretation of the data and in the drafting of the manuscript. A. Mompart-Penina reviewed the analysis and participated in the interpretation of the data. All authors have read and approved the final manuscript.
FundingFor this study funding was provided by the Department of Health (Departament de Salut) of the Government of Catalonia, the Althaia Foundation (Fundació Althaia), Parc Sanitari Sant Joan de Déu and the Catalan Hospital Consortium (Consorci Hospitalari de Catalunya).
Conflict of interestNone declared.
We would like to thank the contributions of the members of the COSTDEP Group and the technical units of the Department of Health. We also thank Cristina Molina and Esther Jorda of the Catalan Department of Health, Juan Cabases and Eduardo Sánchez-Iriso of the Public University of Navarre, Pilar García-Gómez of the Erasmus University, Rotterdam, Delphine Capdevielle of the University of Montpellier and Pedro Enrique Muñoz of PSICOST. The contributions of the members of the following expert groups were invaluable. Experts group A: Pere Bonet, Antoni Bulbena, Miquel Casas, Josep M. Haro, Josefina Jardí, Diego Palao, Víctor Pérez, Josep Ramos and Antoni Serrano. Expert group B: Constança Alberti, Pilar Brugulat, Elena Calvo, Mercè Mercader, Anna Moral, Alba Prat, María J. Pueyo and Roser Vicente (one of the authors of the study, A. Mompart, was also member of this group).