Underreporting of work-related cancer in the Basque Country (Spain) is massive. The aim of our study is to estimate the job-related cancer in the Basque Country in 2008 treated by the Basque Public Health System-Osakidetza, as well as the medical costs derived from its treatment in the same year.
MethodsScientific evidence from industrialised countries is used to estimate the number of processes of cancer attributable to work. Medical costs for specialised care (outpatient and hospital admissions) are derived from the National Health System cost accounts. Costs due to primary health care and pharmaceutical benefits are obtained from Spanish secondary sources. Figures were computed according to disease and sex.
ResultsWe estimate 1,331 work-attributable cancers hospitalizations and 229 work-attributable cancers specialized ambulatory cases. Medical costs borne by public health care system exceed 10 million euros. Specialized care accounts for 64.2% of the total cost. Bronchus and lung cancer represents the largest percentage of total expenditure (27%), followed by the bladder cancer (12.6%), mesothelioma (8.6%), the colon cancer (7.3%), and stomach (6.7%).
ConclusionsThe magnitude of cancer attributable to work in the Basque Country is much higher than reflected in the official Registry of Occupational Diseases. Underreporting of work-related cancers hampers prevention and shifts funding of medical costs from social security to the tax-financed public health system.
La falta de reconocimiento del cáncer como enfermedad profesional en el País Vasco es enorme. Nuestro objetivo es estimar el número de procesos atendidos por cáncer atribuibles al trabajo en el País Vasco en 2008, así como los gastos médicos derivados de su atención en el Servicio Público Vasco de Salud-Osakidetza ese mismo año.
MétodosEl número de procesos se estimó aplicando las fracciones atribuibles al trabajo obtenidas en la literatura científica. Para el cálculo de los costes se utilizaron datos primarios de contabilidad analítica del Sistema Nacional de Salud relativos a la atención especializada (ambulatoria e ingresos hospitalarios), y fuentes secundarias españolas para calcular el coste de la atención primaria de salud y la atención farmacéutica. Los cálculos se realizaron por enfermedad y sexo.
ResultadosEn Osakidetza, en 2008, hubo 1331 hospitalizaciones y 229 consultas a atención ambulatoria especializada debidas a cánceres atribuibles al trabajo. El tratamiento de estos procesos supuso más de 10 millones de euros, de los cuales el 64,2% corresponden a la atención especializada. Por tipo de cáncer, el de bronquio y pulmón, fundamentalmente en hombres, es el que implica mayor gasto sanitario (27%), seguido del de vejiga (12,6%), el mesotelioma (8,6%), el de colon (7,3%) y el de estómago (6,7%).
ConclusionesLa magnitud del cáncer derivado del trabajo en el País Vasco es muy superior a la que refleja el registro de enfermedades profesionales, lo que obstaculiza su prevención y desplaza el correspondiente gasto sanitario del sistema de seguridad social al sistema público de salud.
The reporting of occupational diseases in the Basque Country (Spain) is two to six-fold higher than in other regions of Spain and Europe.1 Under-reporting of occupational cancer, however, is very high. Only 25 work-related cancers were compensated from 1995 to 2008. Among them, 15 have been reported in the last two years: 7 mesothelioma, 4 skin non-melanoma, 2 lymphomas, 1 bronchus and lung and 1 nasal sinuses or nasopharyneal cancer.1 The tumors most commonly reported in the literature as work-related (mostly on industrial workers) are those such as lung, bladder, sinonasal cancer, liver, mesothelioma, leukemia, lymphoma, and non-melanoma skin cancers.2–12
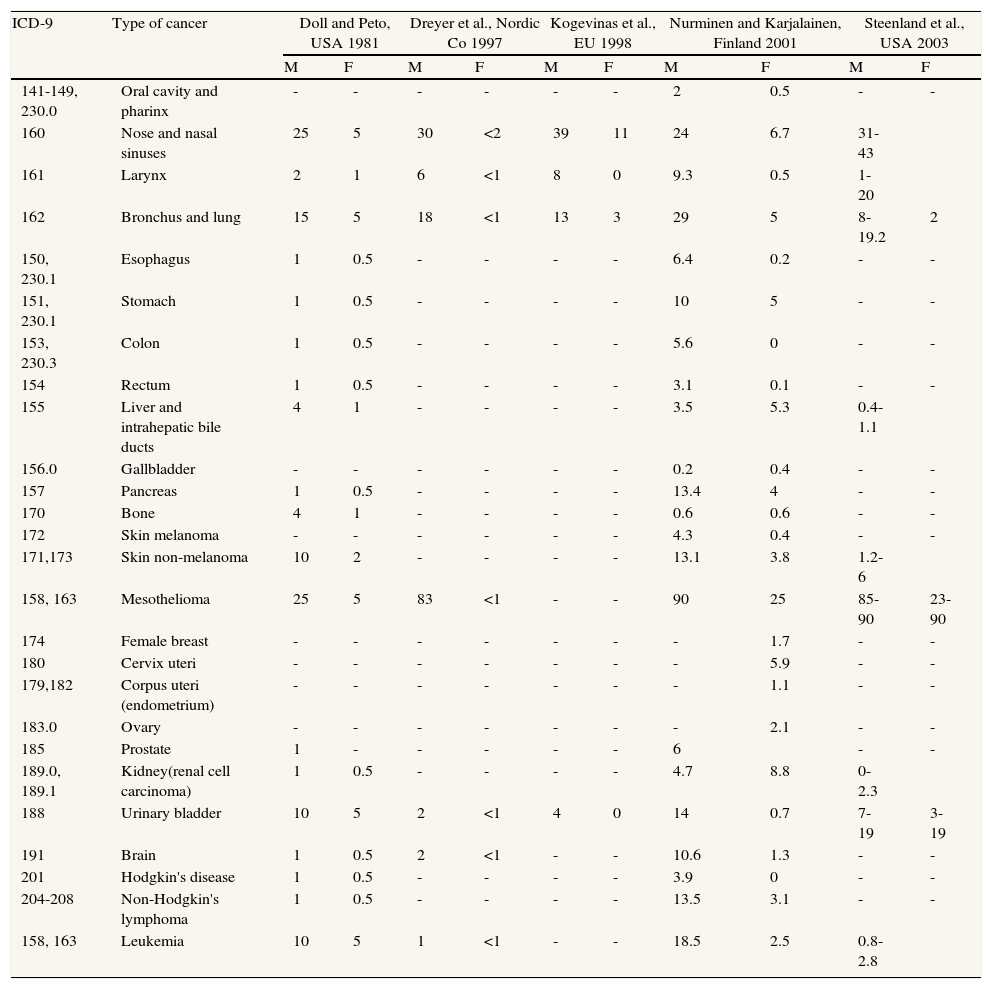
There are many epidemiological studies that evaluate the Spanish population in relation to occupational cancer, and several reviews on occupational cancer in Spain have also been published,13 but it is difficult to obtain a comprehensive estimate of work-related cancers from these studies. Following the lead of others,8,13 we primarily use studies performed in other comparably industrialized countries to obtain a global estimate of work-attributable cancer proportions in Spain (Table 1).4–6,15,16
Matrix of type of cancer, ICD-9 codes, and attributable fractions due to work according to published studies.
| ICD-9 | Type of cancer | Doll and Peto, USA 1981 | Dreyer et al., Nordic Co 1997 | Kogevinas et al., EU 1998 | Nurminen and Karjalainen, Finland 2001 | Steenland et al., USA 2003 | |||||
| M | F | M | F | M | F | M | F | M | F | ||
| 141-149, 230.0 | Oral cavity and pharinx | - | - | - | - | - | - | 2 | 0.5 | - | - |
| 160 | Nose and nasal sinuses | 25 | 5 | 30 | <2 | 39 | 11 | 24 | 6.7 | 31-43 | |
| 161 | Larynx | 2 | 1 | 6 | <1 | 8 | 0 | 9.3 | 0.5 | 1-20 | |
| 162 | Bronchus and lung | 15 | 5 | 18 | <1 | 13 | 3 | 29 | 5 | 8-19.2 | 2 |
| 150, 230.1 | Esophagus | 1 | 0.5 | - | - | - | - | 6.4 | 0.2 | - | - |
| 151, 230.1 | Stomach | 1 | 0.5 | - | - | - | - | 10 | 5 | - | - |
| 153, 230.3 | Colon | 1 | 0.5 | - | - | - | - | 5.6 | 0 | - | - |
| 154 | Rectum | 1 | 0.5 | - | - | - | - | 3.1 | 0.1 | - | - |
| 155 | Liver and intrahepatic bile ducts | 4 | 1 | - | - | - | - | 3.5 | 5.3 | 0.4-1.1 | |
| 156.0 | Gallbladder | - | - | - | - | - | - | 0.2 | 0.4 | - | - |
| 157 | Pancreas | 1 | 0.5 | - | - | - | - | 13.4 | 4 | - | - |
| 170 | Bone | 4 | 1 | - | - | - | - | 0.6 | 0.6 | - | - |
| 172 | Skin melanoma | - | - | - | - | - | - | 4.3 | 0.4 | - | - |
| 171,173 | Skin non-melanoma | 10 | 2 | - | - | - | - | 13.1 | 3.8 | 1.2-6 | |
| 158, 163 | Mesothelioma | 25 | 5 | 83 | <1 | - | - | 90 | 25 | 85-90 | 23-90 |
| 174 | Female breast | - | - | - | - | - | - | - | 1.7 | - | - |
| 180 | Cervix uteri | - | - | - | - | - | - | - | 5.9 | - | - |
| 179,182 | Corpus uteri (endometrium) | - | - | - | - | - | - | - | 1.1 | - | - |
| 183.0 | Ovary | - | - | - | - | - | - | - | 2.1 | - | - |
| 185 | Prostate | 1 | - | - | - | - | - | 6 | - | - | |
| 189.0, 189.1 | Kidney(renal cell carcinoma) | 1 | 0.5 | - | - | - | - | 4.7 | 8.8 | 0-2.3 | |
| 188 | Urinary bladder | 10 | 5 | 2 | <1 | 4 | 0 | 14 | 0.7 | 7-19 | 3-19 |
| 191 | Brain | 1 | 0.5 | 2 | <1 | - | - | 10.6 | 1.3 | - | - |
| 201 | Hodgkin's disease | 1 | 0.5 | - | - | - | - | 3.9 | 0 | - | - |
| 204-208 | Non-Hodgkin's lymphoma | 1 | 0.5 | - | - | - | - | 13.5 | 3.1 | - | - |
| 158, 163 | Leukemia | 10 | 5 | 1 | <1 | - | - | 18.5 | 2.5 | 0.8-2.8 | |
M: male; F: female.
Correctly identifying occupational cancer is a crucial task, not only to protect workers’ health but also for his pocket. Workers receive lower disability payments if the cancer is deemed non-occupational (60% of his/her base salary for the first three weeks and 75% thereafter versus 100% of his/her base salary beginning on the first day for occupational cancers). In addition, free pharmaceutical treatment is provided if the cancer is reported as occupational.
Identification is the first step to prevention. A lot of these cancers do not appear until retirement. As a result, a large part of their costs are covered by the public health system, financed by general taxes, instead of being supported by social contributions (employers and employees contributions to the social security system). In such conditions, the companies responsible for the occupational exposure that caused the disease do not have to pay for the real costs, which will be covered by taxes.
Malignant neoplasias have a major importance, given that they are numerous, the treatment required is expensive, they cause frequent work absences, both short and long term, and may cause premature death or a significant decline in the quality of life. Moreover, certain segments of the population can be more affected than others, causing social inequalities. Finally some cancers can be easily prevented.
From the point of view of the sustainability of the social protection systems, the clarification of the assignments of costs can help to improve the efficiency and efficacy of the social security, occupational risk prevention and health systems. Being aware of the cost of medical care that occupational cancer requires is particularly useful for the sustainability of the public health system, as well as for the adequate management of the prevention system. If these diseases were identified as occupational, they could be included in the global Strategies for Safety and Health at the Workplace, and the specific prevention plans in the associated workplaces, and, thereby, millions of euros would be saved from regional and national budgets.
In this context, our aim is to evaluate the burden of cancer attributable to work in the Basque Country in 2008, as well as the health care costs derived from its treatment in the Basque Public Health System-Osakidetza (SVS-O), using data from the analytic accounting of the National Health System (NHS). We have recently published on the direct health care costs associated with the lung and bladder cancer attributable to work in Spain in 2008.14 We now present the global burden of cancer attributable to work in the Basque Country in 2008.
MethodsThe numbers of occupational cancers in the Basque region in 2008 was derived by applying the estimates of cancer proportions due to occupational exposures, that were obtained from studies performed in other industrialized countries, to the databases with clinic information of various levels of health care of the SVS-O. These estimates do not include associated health costs, but allows their calculation.
Numerous occupational attributable fractions have been developed, including those by Doll and Peto (1981) for the U.S.A. population,4 Dreyer et al. (1997) for the Nordic countries,15 Kogevinas et al. (1998) for Europe,16 Nurminen and Karjalainen (2001) for Finland,6 and Steenland et al. (2003) for the U.S.A.5 (Table 1). Some of the most recent estimates are detailed in United Kingdom,17 indicating that at present occupational exposures continue to cause 4% of all cancers, the same percentage estimated 30 years ago by Doll and Peto. We use the estimations of Nurminen and Karjailainen's for calculation of numbers of occupational cancers and associated health costs for specific cancer type, due to the quality, rigor and completeness of their approach.
Calculation of costs of the diseases was focused on direct health care costs. For its estimation, both primary and secondary data sources related to Spain were used. We use the prevalence approach to estimate the value of health care available to all patients at a time, regardless of when they were diagnosed. Two types of analysis were performed: first, primary data of cost of specialized care by the NHS (hospital and specialized outpatient care) was used to compute costs corresponding to subjects with work attributed cancer who were treated at Basque public hospitals; and second, secondary data sources were used to estimate costs of both primary health care and pharmaceutical care.18 The sources of information used were all Spanish.
Access to the statistics data in the Information System of the NHS was made through NHS Interactive Consultation19 and through the NHS Information Repository20 upon request and being in possession of an electronic signature certificate.
Databases used were record of hospital discharges (CMBD-H) and record of ambulatory specialized attention (CMBD-AAE), and the variables studied were:
- –
Year: 2008.
- –
Hospital location: Basque Country.
- –
Age: 25 or older.
- –
Sex: both.
- –
ICD-9-CM diagnosis: main diagnosis is coded using the ICD-9-MC (International Classification of Diseases, 9th Revision, Clinical Modification). They can be disaggregated up to end of branch (diagnosis coded to 5 digits). This study made consultations with individual diagnosis as search criteria (filter) possible.
- –
Subjects in the CMBD-H: hospital discharges with hospitalization at Basque public hospitals. Exclusions included subjects without a discharge date or if the discharge date was not in 2008; duplicate records; and those corresponding to subjects who were not hospitalized (i.e, they had the same admission and discharge date except on cases of death, transfer or voluntary discharge).
- –
Subjects in the CMBD-AAE: subjects treated (sessions, visits, contacts) in specialized ambulatory attention (AAE) (day hospital, outpatients surgery and specialized home care). Exclusions included those whose date of discharge was not in 2008 or it was inexistent, as well as duplicate records.
- –
Average time of stay: average time of stay in hospital for all subjects.
- –
Average cost: average cost estimated from subjects treated at a representative sample of NHS hospitals for the corresponding year.
- –
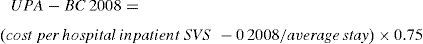
Weighted Activity Unit (in Spanish UPA): unit cost of ambulatory specialized attention adapting the “Weighted Activity Unit” (UPA)21 of the hospital costs per day and disease. It has been estimated as 75% of the cost per day hospital inpatient.22
- –
Weighted Activity Unit in the Basque Country in 2008 (UPA-BC 2008): unit cost for specialized outpatient services in the Basque Country in 2008. Following formula was used to calculate the new variable for the Basque Country:
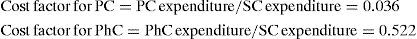
As primary data for the rest of health care costs were not available, we assigned relative weights of primary care and pharmaceutical care costs in relation to costs of specialized care, from data provided by the Government of Catalonia18 (Spain) where the health care budget for the year 2008 is distributed across the 17 relevant disease categories covered by the ICD-9. Disaggregated data are provided for specialized care (SC), primary (PC) and pharmaceutical care (PhC). At our knowledge, this is the only Spanish available source with such a degree of disaggregation. Public expenditure on SC includes inpatient care and specialized outpatient services, while PhC includes expenditure on prescription drugs and also pharmaceutical expenditure supplied for outpatient care at hospitals. In 2008, SC of cancer costs rises to 488,882 thousand euros, PC, 17,745 thousand euros, and PhC, 255,409 thousand euros. From these figures, we have obtained the following cost factors:
These factors were applied afterwards to the specialized care costs for each type of cancer that was calculated with primary sources.
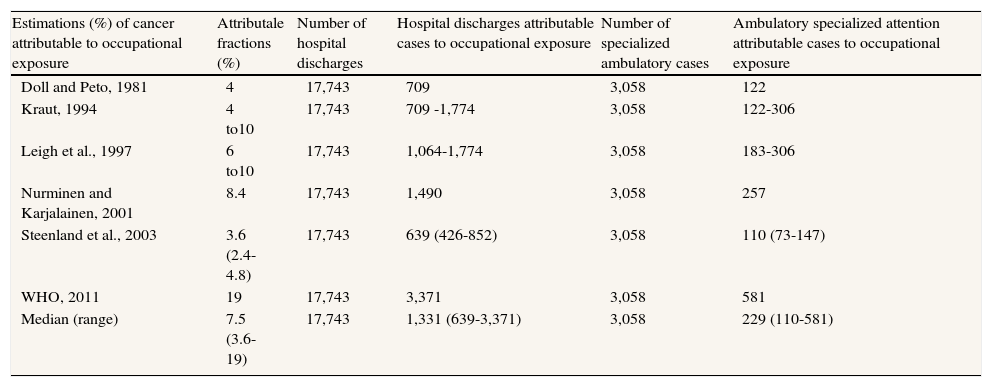
ResultsOne in six (17%) of hospital discharges of people aged 25 years or older in the Basque Country in 2008 were due to cancer. Specifically, 17,743 hospitalizations due to cancer occurred, 9,867 in men and 4,657 in women. Table 2 shows the number of cancer hospital discharges and specialized ambulatory cases (AAE) attributable to work in the Basque Country in 2008, according to the published estimates of cancer proportions attributable to occupation. The estimates of hospital entries range from 639 to 3,371 cases, with a median of 1,331 cases. Patients who received outpatient care for cancers numbered 3,058. Among those, between 110 and 581 with a median of 229, are attributable to work.
Occupational attributale fractions, hospital discharges and specialized ambulatory cases for cancer in the Basque Country, 2008, according to published studies.
| Estimations (%) of cancer attributable to occupational exposure | Attributale fractions (%) | Number of hospital discharges | Hospital discharges attributable cases to occupational exposure | Number of specialized ambulatory cases | Ambulatory specialized attention attributable cases to occupational exposure |
| Doll and Peto, 1981 | 4 | 17,743 | 709 | 3,058 | 122 |
| Kraut, 1994 | 4 to10 | 17,743 | 709 -1,774 | 3,058 | 122-306 |
| Leigh et al., 1997 | 6 to10 | 17,743 | 1,064-1,774 | 3,058 | 183-306 |
| Nurminen and Karjalainen, 2001 | 8.4 | 17,743 | 1,490 | 3,058 | 257 |
| Steenland et al., 2003 | 3.6 (2.4-4.8) | 17,743 | 639 (426-852) | 3,058 | 110 (73-147) |
| WHO, 2011 | 19 | 17,743 | 3,371 | 3,058 | 581 |
| Median (range) | 7.5 (3.6-19) | 17,743 | 1,331 (639-3,371) | 3,058 | 229 (110-581) |
Source: own elaboration by interactive consultation in the National Health System and National Health System Database. Institute of Sanitary Information. Ministry of Health, Social Policy and Equity [access April 2011]. Available from: http://pestadistico.msc.es and http://repositorio.msc.es/risns/.
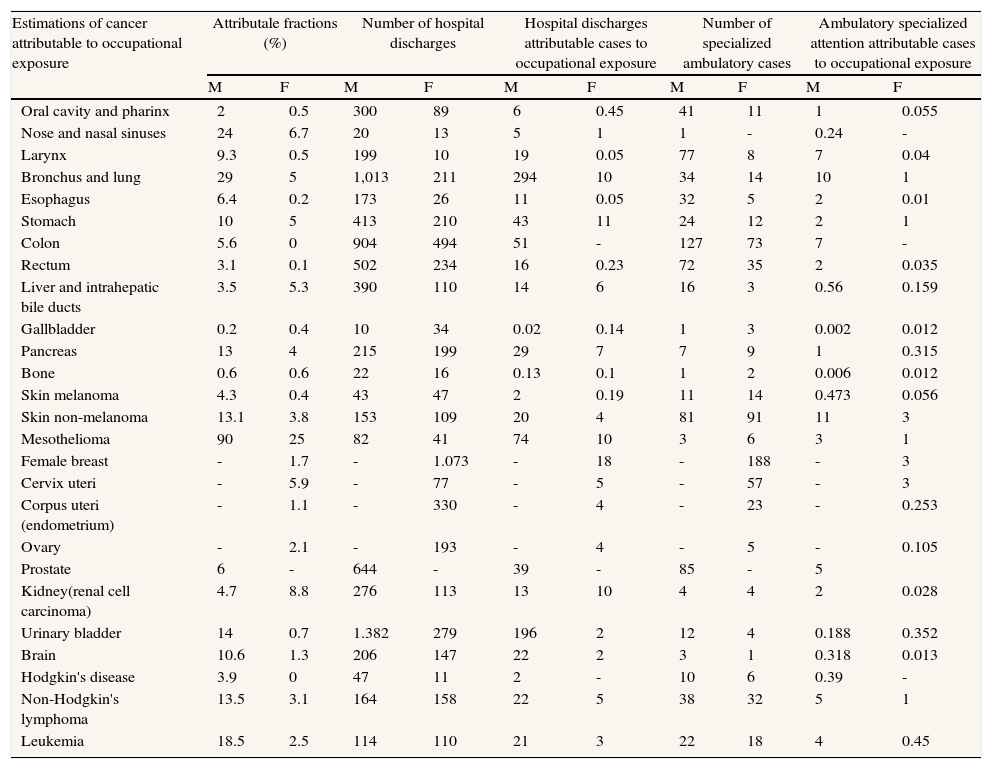
Table 3 shows the number of hospital discharges by cancer site and sex, and the cases that, among them, are attributable to work, using Nurminen and Karjalainen attributable fraction estimates. The most frequent cancers attributable to work among men are lung and bladder, followed by mesothelioma. Among women, the most frequent cancers attributable to work are breast and stomach cancer, followed by lung, mesothelioma and kidney.
Hospital discharges per type of cancer and sex, in the Basque Country in 2008 attributable to occupational exposures according to Nurninen and Karjalainen estimates (2001).
| Estimations of cancer attributable to occupational exposure | Attributale fractions (%) | Number of hospital discharges | Hospital discharges attributable cases to occupational exposure | Number of specialized ambulatory cases | Ambulatory specialized attention attributable cases to occupational exposure | |||||
| M | F | M | F | M | F | M | F | M | F | |
| Oral cavity and pharinx | 2 | 0.5 | 300 | 89 | 6 | 0.45 | 41 | 11 | 1 | 0.055 |
| Nose and nasal sinuses | 24 | 6.7 | 20 | 13 | 5 | 1 | 1 | - | 0.24 | - |
| Larynx | 9.3 | 0.5 | 199 | 10 | 19 | 0.05 | 77 | 8 | 7 | 0.04 |
| Bronchus and lung | 29 | 5 | 1,013 | 211 | 294 | 10 | 34 | 14 | 10 | 1 |
| Esophagus | 6.4 | 0.2 | 173 | 26 | 11 | 0.05 | 32 | 5 | 2 | 0.01 |
| Stomach | 10 | 5 | 413 | 210 | 43 | 11 | 24 | 12 | 2 | 1 |
| Colon | 5.6 | 0 | 904 | 494 | 51 | - | 127 | 73 | 7 | - |
| Rectum | 3.1 | 0.1 | 502 | 234 | 16 | 0.23 | 72 | 35 | 2 | 0.035 |
| Liver and intrahepatic bile ducts | 3.5 | 5.3 | 390 | 110 | 14 | 6 | 16 | 3 | 0.56 | 0.159 |
| Gallbladder | 0.2 | 0.4 | 10 | 34 | 0.02 | 0.14 | 1 | 3 | 0.002 | 0.012 |
| Pancreas | 13 | 4 | 215 | 199 | 29 | 7 | 7 | 9 | 1 | 0.315 |
| Bone | 0.6 | 0.6 | 22 | 16 | 0.13 | 0.1 | 1 | 2 | 0.006 | 0.012 |
| Skin melanoma | 4.3 | 0.4 | 43 | 47 | 2 | 0.19 | 11 | 14 | 0.473 | 0.056 |
| Skin non-melanoma | 13.1 | 3.8 | 153 | 109 | 20 | 4 | 81 | 91 | 11 | 3 |
| Mesothelioma | 90 | 25 | 82 | 41 | 74 | 10 | 3 | 6 | 3 | 1 |
| Female breast | - | 1.7 | - | 1.073 | - | 18 | - | 188 | - | 3 |
| Cervix uteri | - | 5.9 | - | 77 | - | 5 | - | 57 | - | 3 |
| Corpus uteri (endometrium) | - | 1.1 | - | 330 | - | 4 | - | 23 | - | 0.253 |
| Ovary | - | 2.1 | - | 193 | - | 4 | - | 5 | - | 0.105 |
| Prostate | 6 | - | 644 | - | 39 | - | 85 | - | 5 | |
| Kidney(renal cell carcinoma) | 4.7 | 8.8 | 276 | 113 | 13 | 10 | 4 | 4 | 2 | 0.028 |
| Urinary bladder | 14 | 0.7 | 1.382 | 279 | 196 | 2 | 12 | 4 | 0.188 | 0.352 |
| Brain | 10.6 | 1.3 | 206 | 147 | 22 | 2 | 3 | 1 | 0.318 | 0.013 |
| Hodgkin's disease | 3.9 | 0 | 47 | 11 | 2 | - | 10 | 6 | 0.39 | - |
| Non-Hodgkin's lymphoma | 13.5 | 3.1 | 164 | 158 | 22 | 5 | 38 | 32 | 5 | 1 |
| Leukemia | 18.5 | 2.5 | 114 | 110 | 21 | 3 | 22 | 18 | 4 | 0.45 |
M: male; F: female.
Source: own elaboration from National Health System Database. Institute of Sanitary Information. Ministry of Health, Social Policy and Equity [access April 2011]. Available from: http://repositorio.msc.es/risns/.
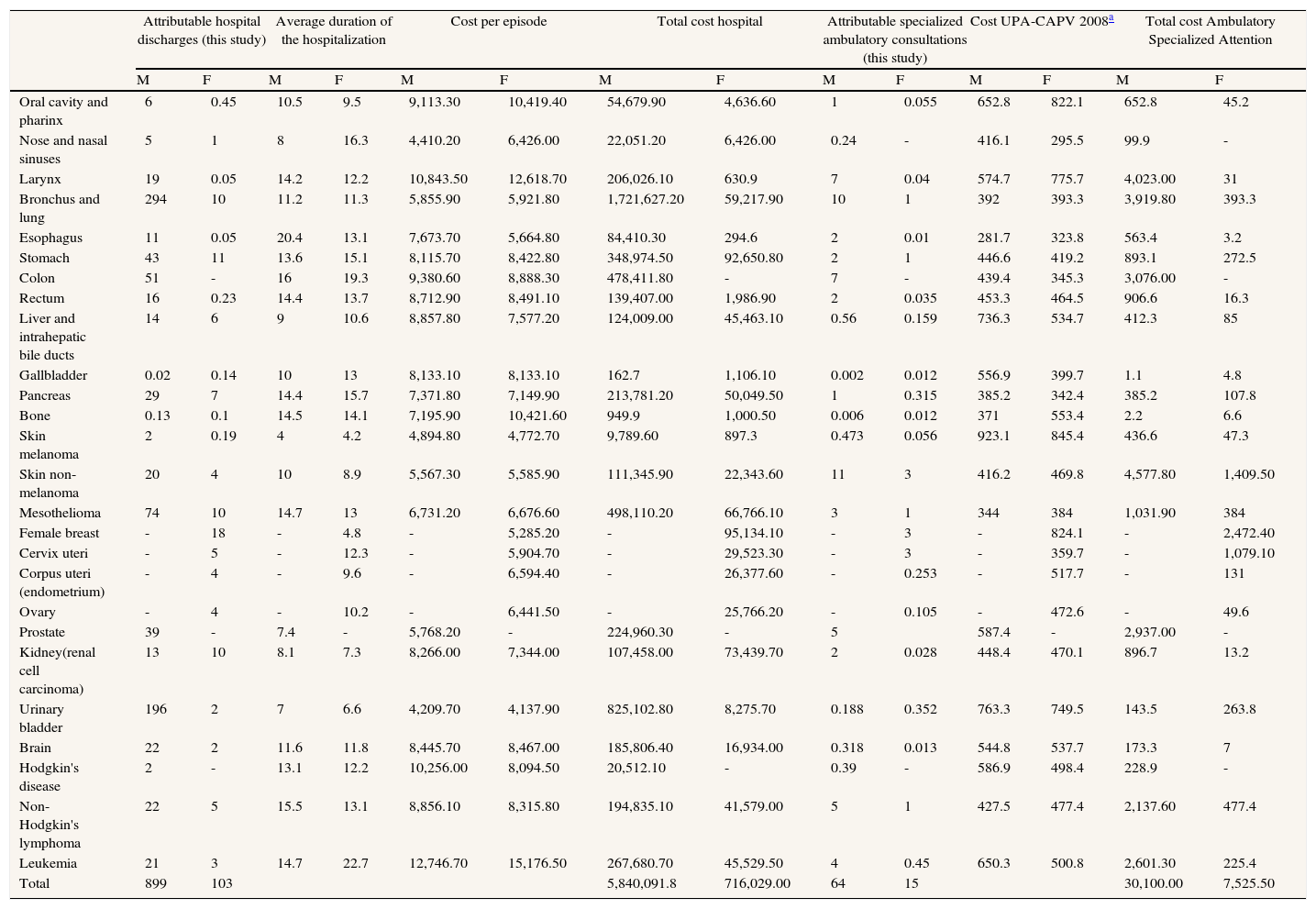
The costs associated with hospital discharges of patients with work- related cancers paid by the Basque Public Health System are shown in Table 4 and total 6,556,120.9 € in 2008. These costs are eight-fold higher in men than in women due to the more frequent occurrence of occupational cancer in men than in women.
Costs of specialized ambulatory cases of cancer attributable to occupational exposure in Basque Country in 2008 (euros).
| Attributable hospital discharges (this study) | Average duration of the hospitalization | Cost per episode | Total cost hospital | Attributable specialized ambulatory consultations (this study) | Cost UPA-CAPV 2008a | Total cost Ambulatory Specialized Attention | ||||||||
| M | F | M | F | M | F | M | F | M | F | M | F | M | F | |
| Oral cavity and pharinx | 6 | 0.45 | 10.5 | 9.5 | 9,113.30 | 10,419.40 | 54,679.90 | 4,636.60 | 1 | 0.055 | 652.8 | 822.1 | 652.8 | 45.2 |
| Nose and nasal sinuses | 5 | 1 | 8 | 16.3 | 4,410.20 | 6,426.00 | 22,051.20 | 6,426.00 | 0.24 | - | 416.1 | 295.5 | 99.9 | - |
| Larynx | 19 | 0.05 | 14.2 | 12.2 | 10,843.50 | 12,618.70 | 206,026.10 | 630.9 | 7 | 0.04 | 574.7 | 775.7 | 4,023.00 | 31 |
| Bronchus and lung | 294 | 10 | 11.2 | 11.3 | 5,855.90 | 5,921.80 | 1,721,627.20 | 59,217.90 | 10 | 1 | 392 | 393.3 | 3,919.80 | 393.3 |
| Esophagus | 11 | 0.05 | 20.4 | 13.1 | 7,673.70 | 5,664.80 | 84,410.30 | 294.6 | 2 | 0.01 | 281.7 | 323.8 | 563.4 | 3.2 |
| Stomach | 43 | 11 | 13.6 | 15.1 | 8,115.70 | 8,422.80 | 348,974.50 | 92,650.80 | 2 | 1 | 446.6 | 419.2 | 893.1 | 272.5 |
| Colon | 51 | - | 16 | 19.3 | 9,380.60 | 8,888.30 | 478,411.80 | - | 7 | - | 439.4 | 345.3 | 3,076.00 | - |
| Rectum | 16 | 0.23 | 14.4 | 13.7 | 8,712.90 | 8,491.10 | 139,407.00 | 1,986.90 | 2 | 0.035 | 453.3 | 464.5 | 906.6 | 16.3 |
| Liver and intrahepatic bile ducts | 14 | 6 | 9 | 10.6 | 8,857.80 | 7,577.20 | 124,009.00 | 45,463.10 | 0.56 | 0.159 | 736.3 | 534.7 | 412.3 | 85 |
| Gallbladder | 0.02 | 0.14 | 10 | 13 | 8,133.10 | 8,133.10 | 162.7 | 1,106.10 | 0.002 | 0.012 | 556.9 | 399.7 | 1.1 | 4.8 |
| Pancreas | 29 | 7 | 14.4 | 15.7 | 7,371.80 | 7,149.90 | 213,781.20 | 50,049.50 | 1 | 0.315 | 385.2 | 342.4 | 385.2 | 107.8 |
| Bone | 0.13 | 0.1 | 14.5 | 14.1 | 7,195.90 | 10,421.60 | 949.9 | 1,000.50 | 0.006 | 0.012 | 371 | 553.4 | 2.2 | 6.6 |
| Skin melanoma | 2 | 0.19 | 4 | 4.2 | 4,894.80 | 4,772.70 | 9,789.60 | 897.3 | 0.473 | 0.056 | 923.1 | 845.4 | 436.6 | 47.3 |
| Skin non-melanoma | 20 | 4 | 10 | 8.9 | 5,567.30 | 5,585.90 | 111,345.90 | 22,343.60 | 11 | 3 | 416.2 | 469.8 | 4,577.80 | 1,409.50 |
| Mesothelioma | 74 | 10 | 14.7 | 13 | 6,731.20 | 6,676.60 | 498,110.20 | 66,766.10 | 3 | 1 | 344 | 384 | 1,031.90 | 384 |
| Female breast | - | 18 | - | 4.8 | - | 5,285.20 | - | 95,134.10 | - | 3 | - | 824.1 | - | 2,472.40 |
| Cervix uteri | - | 5 | - | 12.3 | - | 5,904.70 | - | 29,523.30 | - | 3 | - | 359.7 | - | 1,079.10 |
| Corpus uteri (endometrium) | - | 4 | - | 9.6 | - | 6,594.40 | - | 26,377.60 | - | 0.253 | - | 517.7 | - | 131 |
| Ovary | - | 4 | - | 10.2 | - | 6,441.50 | - | 25,766.20 | - | 0.105 | - | 472.6 | - | 49.6 |
| Prostate | 39 | - | 7.4 | - | 5,768.20 | - | 224,960.30 | - | 5 | 587.4 | - | 2,937.00 | - | |
| Kidney(renal cell carcinoma) | 13 | 10 | 8.1 | 7.3 | 8,266.00 | 7,344.00 | 107,458.00 | 73,439.70 | 2 | 0.028 | 448.4 | 470.1 | 896.7 | 13.2 |
| Urinary bladder | 196 | 2 | 7 | 6.6 | 4,209.70 | 4,137.90 | 825,102.80 | 8,275.70 | 0.188 | 0.352 | 763.3 | 749.5 | 143.5 | 263.8 |
| Brain | 22 | 2 | 11.6 | 11.8 | 8,445.70 | 8,467.00 | 185,806.40 | 16,934.00 | 0.318 | 0.013 | 544.8 | 537.7 | 173.3 | 7 |
| Hodgkin's disease | 2 | - | 13.1 | 12.2 | 10,256.00 | 8,094.50 | 20,512.10 | - | 0.39 | - | 586.9 | 498.4 | 228.9 | - |
| Non-Hodgkin's lymphoma | 22 | 5 | 15.5 | 13.1 | 8,856.10 | 8,315.80 | 194,835.10 | 41,579.00 | 5 | 1 | 427.5 | 477.4 | 2,137.60 | 477.4 |
| Leukemia | 21 | 3 | 14.7 | 22.7 | 12,746.70 | 15,176.50 | 267,680.70 | 45,529.50 | 4 | 0.45 | 650.3 | 500.8 | 2,601.30 | 225.4 |
| Total | 899 | 103 | 5,840,091.8 | 716,029.00 | 64 | 15 | 30,100.00 | 7,525.50 | ||||||
Source: own elaboration from National Health System Database. Institute of Sanitary Information. Ministry of Health, Social Policy and Equity [access April 2011]. Available from: http://repositorio.msc.es/risns/.
The work-related cancers that involve the highest cost to the Basque Public Health System per hospital entry are lung, bladder, mesothelioma, colon, stomach and leukemia. By sex, the cost attributable to male treatment ranges from 79% (stomach cancer) to 99% (bladder cancer), while the lowest cost goes from 13% (gallbladder cancer) to 48% (bone cancer), plus colon and Hodgkin cancers, with all the costs attributed to male treatment.
Although the mean cost per hospitalization is higher for men in almost all the cancers, if we look at the average cost, women show higher values for bone cancer, sinonasal, breast cancer, oral cavity and pharinx, larynx, leukemia, stomach and lung. Also, the average duration of the hospitalization is higher for women than men when suffering from nose and nasal sinuses cancers, stomach, liver and intrahepatic bile ducts, gallbladder, pancreas and leukemia.
The total costs of specialized outpatients care cancer are 37,625.50 €. Costs of AAE care for work-related cancer is fourfold higher in men than in women. Cancers with the overall highest AAE-associated costs are skin cancer (non-melanoma), lung and larynx.
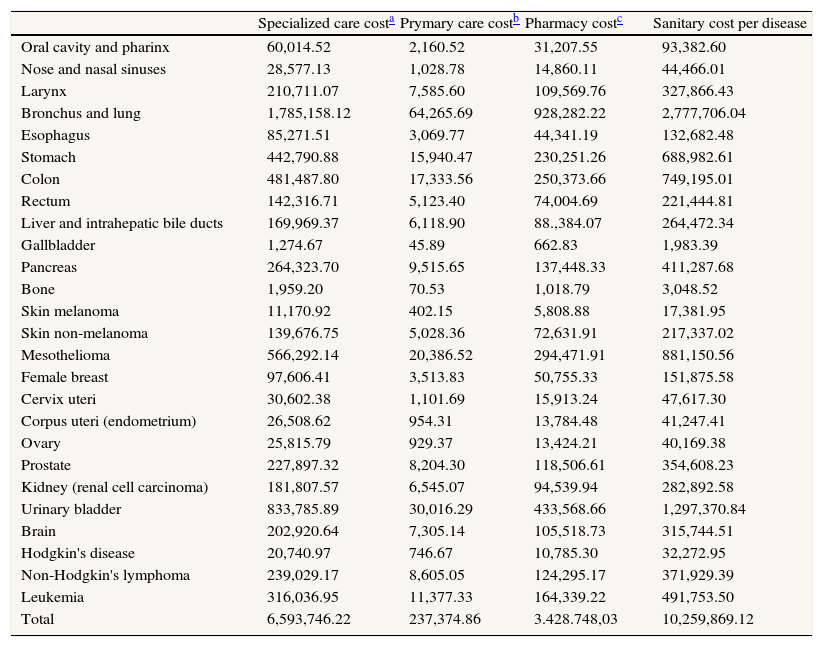
The total specialized care cost of illness is the sum of the costs of hospital admissions, day hospital, day surgery and home care (AAE) costs. Summing these items in Table 4, the total value is 6,593,746 €. When analyzed individually and for both sexes, lung (27%), bladder (12.6%), mesothelioma (8%), colon (8,6%), and stomach (6,7%) are those with the highest hospital-related costs (Table 5).
Total sanitary costs per type of occupational cancer in Basque Country in 2008 (euros).
| Specialized care costa | Prymary care costb | Pharmacy costc | Sanitary cost per disease | |
| Oral cavity and pharinx | 60,014.52 | 2,160.52 | 31,207.55 | 93,382.60 |
| Nose and nasal sinuses | 28,577.13 | 1,028.78 | 14,860.11 | 44,466.01 |
| Larynx | 210,711.07 | 7,585.60 | 109,569.76 | 327,866.43 |
| Bronchus and lung | 1,785,158.12 | 64,265.69 | 928,282.22 | 2,777,706.04 |
| Esophagus | 85,271.51 | 3,069.77 | 44,341.19 | 132,682.48 |
| Stomach | 442,790.88 | 15,940.47 | 230,251.26 | 688,982.61 |
| Colon | 481,487.80 | 17,333.56 | 250,373.66 | 749,195.01 |
| Rectum | 142,316.71 | 5,123.40 | 74,004.69 | 221,444.81 |
| Liver and intrahepatic bile ducts | 169,969.37 | 6,118.90 | 88.,384.07 | 264,472.34 |
| Gallbladder | 1,274.67 | 45.89 | 662.83 | 1,983.39 |
| Pancreas | 264,323.70 | 9,515.65 | 137,448.33 | 411,287.68 |
| Bone | 1,959.20 | 70.53 | 1,018.79 | 3,048.52 |
| Skin melanoma | 11,170.92 | 402.15 | 5,808.88 | 17,381.95 |
| Skin non-melanoma | 139,676.75 | 5,028.36 | 72,631.91 | 217,337.02 |
| Mesothelioma | 566,292.14 | 20,386.52 | 294,471.91 | 881,150.56 |
| Female breast | 97,606.41 | 3,513.83 | 50,755.33 | 151,875.58 |
| Cervix uteri | 30,602.38 | 1,101.69 | 15,913.24 | 47,617.30 |
| Corpus uteri (endometrium) | 26,508.62 | 954.31 | 13,784.48 | 41,247.41 |
| Ovary | 25,815.79 | 929.37 | 13,424.21 | 40,169.38 |
| Prostate | 227,897.32 | 8,204.30 | 118,506.61 | 354,608.23 |
| Kidney (renal cell carcinoma) | 181,807.57 | 6,545.07 | 94,539.94 | 282,892.58 |
| Urinary bladder | 833,785.89 | 30,016.29 | 433,568.66 | 1,297,370.84 |
| Brain | 202,920.64 | 7,305.14 | 105,518.73 | 315,744.51 |
| Hodgkin's disease | 20,740.97 | 746.67 | 10,785.30 | 32,272.95 |
| Non-Hodgkin's lymphoma | 239,029.17 | 8,605.05 | 124,295.17 | 371,929.39 |
| Leukemia | 316,036.95 | 11,377.33 | 164,339.22 | 491,753.50 |
| Total | 6,593,746.22 | 237,374.86 | 3.428.748,03 | 10,259,869.12 |
Source: own elaboration from National Health System Database. Institute of Sanitary Information. Ministry of Health, Social Policy and Equity [access April 2011]. Available from: http://repositorio.msc.es/risns/.
Table 5 provides the costs of specialized care (hospital discharges and AAE), and the estimates costs of primary health care and pharmaceutical care of work-related cancers, using the cost factors (relative weights) primary care (PC) and pharmaceutical care (PhC) cost factors, as described in the Methods section.
We estimate that the total cost of work-related cancers, in people 25 or older, for the Basque Public Health System in 2008, is 10.26 million euros. It represents 8.54% of total Basque public expenditure on cancer (120.15 million euros) in that year. Hospital-related costs account for two-thirds (64.2%), followed by pharmaceutical costs (33.5%), while primary care plays a marginal role in the neoplasias cost (2.3%) (Table 5). The most costly cancers are cancer of bronchus and lung (27%), mainly in men, followed by bladder (12.6%), mesothelioma (8.6%), colon (7.3%) and stomach (6.7%).
DiscussionIn 2008, 1,331 hospital discharges of people 25 years or older have occurred due to cancer attributable to work in the Basque Public Health System. By contrast, 11 cases of occupational cancers were reported by the social security system in 2008 (5 mesothelioma, 3 non-melanoma skin cancers, 1 lymphoma, 1 lung and 1 sinonasal cancer).1 These data contrast remarkably with even the most conservative estimates of work-related cancers.
The ineffectiveness of the health care and compensation systems for recognizing occupational diseases, specifically cancer, is well-documented. Studies performed in Spain demonstrate this underreporting. Fernández Ajuria et al. studied occupational mortality in the Basque Country in 1987 and found 8 pleural mesotheliomas reported in the Basque Cancer Registry, but only 2 had been evaluated in the Disabilities Medical Assessment Units, and none were recognize as occupational by the social security system,23 while pleural mesothelioma is an occupational health event inherent to work, and it is highly unlikely to develop without an occupational exposure. García and Gadea (2007) estimate the work-related deaths caused by malignant neoplasias in the Basque Country in 2004 to be 460.24 It has also been estimated that 25.4% of the Spanish working population in 2004 was exposed to carcinogens at their workplace.13
Reasons for under-reporting are legion and include the classification of occupational diseases as common diseases, the intrinsic scientific difficulty to catalogue a disease as occupational,25 the ignorance of the health care professionals about occupational risk factors,26 the disinterest in prevention by the health care system, and the resistance by employers to accept the classification of a disease as work-related.27
To estimate the burden of work-related cancer, we have used the published estimations of attributable fractions, specifically those of Leigh et al.,28 Doll and Peto (1981),4 Steenland et al.5 for the U.S. population; the estimates for the Nordic countries,15 and for the Finland;6 and estimates for Europe16 and by WHO (WHO, 2011).29 As we said in the introduction, there are many Spanish epidemiological studies that evaluate the population in relation to occupational cancer, but it is difficult to obtain attributable fractions from these studies. This fact, coupled with the poor quality of the system of occupational cancer, justifies the use of other studies. The estimates vary in large part due to incomplete data, but are nonetheless useful, recognizing limitations. The utilization of attributable fractions in studies performed in other countries may be a limitation of our study, although they have been used in other economically advanced countries.30,31 To be conservative, we use the median value of a wide range of work-attributable fractions. We also used the organ-specific estimates for cancer from the most complete and rigorous analysis of this issue, the study from Finland.6 Even so, not all cancers are included in the Finnish study, and it is likely that we underestimated the number of cases of work-attributable cancers.
As in other studies,8,13 we have found that most work-related cancers occur in men, and that lung and urinary bladder cancers are the most frequent cancers. There is an awareness of the existence of many agents associated to these two cancers, including asbestos, silica, metals, radiation, combustion products, aromatic amines, and other exposures. Other important occupational cancers are mesothelioma, caused almost exclusively by exposure to asbestos, sinonasal cancer, caused by exposure to wood dust, metals and formaldehyde, and leukemia and lymphoma, caused by solvents, insecticides and other chemicals.
Regarding to medical costs generated by these cases of occupational cancer, we chose the prevalence approach to estimate the value of health care available to all patients at a time, regardless of when they were diagnosed,32–34 because it permits analysis of reliable available data that require fewer forecasting assumptions than the incidence method. It must also be emphasized that the sources of information used were all Spanish. We use as a primary source the data from the analytical accounting of the NHS to calculate the health care cost of occupational cancers attended by the Basque Public Health System. We analyzed the direct health costs, which include the medical services used for diagnosis and treatment of the disease. We did not analyze the indirect costs, which correspond to the productivity losses caused by the premature mortality and morbidity associated with these neoplasias, as well as those from the corresponding sick leaves (both temporary and permanent). Non-health costs such as remunerated and non-remunerated caregivers have not been included either. Additionally, only those cancers with enough scientific evidence of their occupational origin have been considered. This is, therefore, an underestimate of the total direct health care costs of work-related cancers. Even so, work-related cancers account for more than 10 million euros, or 8.54% of total Basque public expenditure on cancer care in 2008.
The limitations of our calculation of the costs of occupational cancer are related to the completeness of the primary data on the cost of specialized care and the use of secondary sources for the computation of the primary care and pharmaceutical costs. Regarding the primary sources the coverage of the information system for hospitalizations is 100%. While in the cases attended in ambulatory specialized attention (AAE), the coverage is 100% for the surgical activity, but only 46.7% in the medical activity of the day hospital, according to the Statistics of Sanitary Establishments.22
This limitation leads to an underestimation of the total expenditure for these diseases, which is amplified in calculating costs of primary care and pharmaceutical treatment, since calculation of the latter are based in part on the former. As described in the Methods section, we have combined primary and secondary sources due to the lack of primary sources for all the components of the direct costs.34 It must be emphasized that the difficulties to access primary data are not exclusive for Spain. Other countries show a similar situation. Thus, a Commission of the French Senate responsible for a report similar to this study acknowledged the lack of a database that included the health costs according to diseases and which permitted a reliable calculation of the costs of work related diseases.35 In our view, the use of the Catalonian Health Budget for the same year minimizes these errors, since their reflect figures from one of the Spanish regions. However, when using data from Catalonia as a base for the Basque Country we are assuming that there are no substantial differences between the health care costs structure in both regions. Nevertheless, several authors have pointed to the variability in health care costs across the Spanish NHS, which could be due to differences in factor prices, productivity, efficiency or inappropriate use of services, among other factors.36,37
An advantage of our method was that estimates were derived from linear calculations, which we have attempted with transparency. As a result, any estimate in our tables can be adjusted for a different region in Spain or for a different attributable fraction.
Carcinogens at the workplace play an important role on the identification and prevention of all the carcinogens,2 as they were the first identified and represent a high percentage of the total. All the cancers they cause are preventable. It is important to identify and prevent the carcinogens at workplaces, because the advantages of identification and adequate proceeding benefit the society as a whole, as the general population is also exposed to these substances (for instance, benzene, asbestos, diesel motors exhausts, etc.).
Most diseases, including cancers, are not recognized as occupational diseases even if they result from occupational exposures. Evaluating the under-recognition of occupational diseases remains complex, since the only data available are communicated by social security funds that only take into account the very few cases that effectively led to indemnification. Cancer is a paradigmatic case of this, as can be derived from its minimal reporting as occupational disease, as shown in this paper. This highly impedes the prevention of occupational cancer, given that identification is one of the main issues for its adequate management.
Moreover, the treatment of occupational cancers leads to substantial health care costs which are currently shifted from the social security system to the tax-financed public health system. An important consequence of this transfer is that the companies, which are responsible for conditions that led to the cancers, do not have to pay associated costs and, further, have no incentive to take preventive actions to reduce risk of cancer. The public health system is burdened by this transfer of costs.
The magnitude of the occupational health burden is very large and, therefore, involves a high cost to workers, employers and society as a whole. However, there is a serious problem in Spain with the recognition of occupational cancers. Although the Spanish list of occupational diseases includes many agents that are associated with certain types of cancer, the number of those recognized as professionals is virtually nonexistent. In the past few years the economics of occupational health area has emerged as a key area of research.
What does this study add to the literature?This is the first study in Spain that estimates the burden of cancer attributable to work in the Basque Country in 2008, as well as the health care costs derived from its treatment in the Basque Public Health System-Osakidetza. The sources of information used were all Spanish. Economic evaluation is clearly relevant for future preventive and health promotion programs. This paper will provide information to demonstrate to decision makers in companies and government the necessity for workplaces interventions and adequate provisions of occupational health services. Furthermore, it will show how a proportion of medical costs are being shifted from social security to the tax-financed public health system.
All the authors contributed equally to the conception and design of the study, analysis and interpretation of the data, and drafting and critical review of the manuscript. All the authors have approved the final version for publication.
FundingBasque Institute of Occupational Safety and Health at Work-OSALAN, Bilbao, Spain.
Conflicts of interestNone.