The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
Más datosThe study explored determinant factors of weight status among children aged 12–24 months who received complementary feeding program of the Ministry of Health in Luwu Timur, South Sulawesi Province.
MethodsThe study used case–control design. It involved 82 children from poor families who received complementary feeding program. Forty-one children as a case group with constant body weight and forty-one children as a control group with increasing body weight within the last two months selected with a purposive sampling technique.
ResultsExclusive breastfeeding (OR=3.485; 95% CI=1.380–8.798), the duration of complementary feeding consumption (OR=0.299; 95% CI=0.095–0.939), history of diarrhea (OR=3.071; 95% CI=1.174–8.028) and milk consumption pattern (OR=0.233; 95% CI=0.069–0.791) were significant determinant of body weight status. Exclusive breastfeeding was the most dominant variable for body weight status (B=6.152).
ConclusionsExclusive breastfeeding during the first six months is crucial to support complementary feeding programs in increasing the body weight status of children aged 12–24 months.
The nutritional problem among children under two years old in Indonesia remains a public health concern. The prevalence of undernutrition is still high and spread in several provinces in Indonesia.1,2 One of the regions of Indonesia that are facing nutritional status problems is South Sulawesi Province. The prevalence of undernutrition is 19.6% which was found to be higher than the national figure.1
The impact that occurs if the nutrition of children under five is not fulfilled affect subsequent growth and development of children under five, inhibit cognitive development and increase the risk of under-five mortality. Toddlers who are malnourished are unable to form antibodies (resistance) against infectious diseases as a result of which children often get diseases that interfere with their growth.3
As a follow-up to Global Strategy for Infant and Young Child Feeding.4,5 Indonesian government has set priority health efforts to improve community nutrition, to reduce the prevalence of malnutrition. One of them is through the complementary feeding of breast milk (MP-ASI) programs, especially for children under five from poor families who experience malnutrition. The program is intended to comply the nutritional adequacy of children under five by providing additional food for toddlers, and not to replace the main daily diet for toddlers. One form of MP-ASI program that has been running is in the form of biscuits package which are distributed by the central government to all districts in Indonesia.
The East Luwu Health Office has also received and distributed complementary feeding to sub-districts in its working area, including Mangkutana Sub District, to children aged 6–24 months from poor families who suffer undernutrition. After carrying out the program, it is hoped that the nutritional status of children under-two years will be better by seeing their weight gain. However, there are children who did not gain weight after receiving MP-ASI program.
A preliminary study was conducted in November 2019 showed that of all sub-district, the highest prevalence of children did not reach weight gain within two consecutive months was found in Mangkutana sub-district of 31.58%. Based on this background, the study explored determinant factors that influence body weight among children aged 12–24 months who received MP-ASI program.
MethodsThe study used a case–control design. It was conducted in Mangkutana Sub District, East Luwu Regency, South Sulawesi Province, Indonesia. The population was children aged 12–24 months who received the MP-ASI program from the Ministry of Health in the form of biscuits 120g/day within three months. The study involved 82 children from poor families which were divided equally into case and control groups by matching age chosen through purposive sampling. Case group consists of children who did not reach weight gain, and control group consists of children who reach weight gain within two consecutive months.
Variables collected from mothers were history of giving exclusive breastfeeding (EBF), the duration of consumption of MP-ASI, history of diarrhea using a questionnaire. Children's food consumption focused on the frequency of staple food, dairy, grain, fruits, vegetables, and milk consumption using a food frequency questionnaire. Before implemented, questionnaires were tested to ensure its validity. Information on children's weight status based on recording on children's health books from integrated health services. Data collection was performed through the home visit.
The statistical analysis was carried out using SPSS. The analysis was conducted on two levels. First, a bivariate analysis was performed to determine the constant weights under two years according to explanatory variables. A Chi-square statistic is used to test the relationship between constant weight and risk factors. Secondly, the significant variables (p-value<0.05) observed in bivariate analysis were included in the multivariate analysis by a logistic regression model.
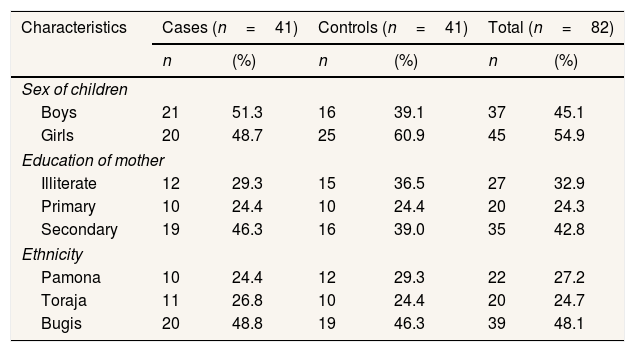
ResultsA total of 82 children below the age of two (41 with constant weight and 41 with weight gain within two months) were analyzed. The mean age of case and control group were 18.1 (±10.2) and 19.5 (±11.6) months, respectively. There were 51.3% of boys in the cases and 39.1% in the controls. All of the mothers in cases and controls were housewives with no occupation. The majority of mother's education (42.8%) were secondary. Secondary education of mothers was higher among cases than in controls. Bugis (48.1%) were the highest ethnicity than Pamona and Toraja (Table 1).
Socio-demographic characteristics of the study population.
| Characteristics | Cases (n=41) | Controls (n=41) | Total (n=82) | |||
|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | |
| Sex of children | ||||||
| Boys | 21 | 51.3 | 16 | 39.1 | 37 | 45.1 |
| Girls | 20 | 48.7 | 25 | 60.9 | 45 | 54.9 |
| Education of mother | ||||||
| Illiterate | 12 | 29.3 | 15 | 36.5 | 27 | 32.9 |
| Primary | 10 | 24.4 | 10 | 24.4 | 20 | 24.3 |
| Secondary | 19 | 46.3 | 16 | 39.0 | 35 | 42.8 |
| Ethnicity | ||||||
| Pamona | 10 | 24.4 | 12 | 29.3 | 22 | 27.2 |
| Toraja | 11 | 26.8 | 10 | 24.4 | 20 | 24.7 |
| Bugis | 20 | 48.8 | 19 | 46.3 | 39 | 48.1 |
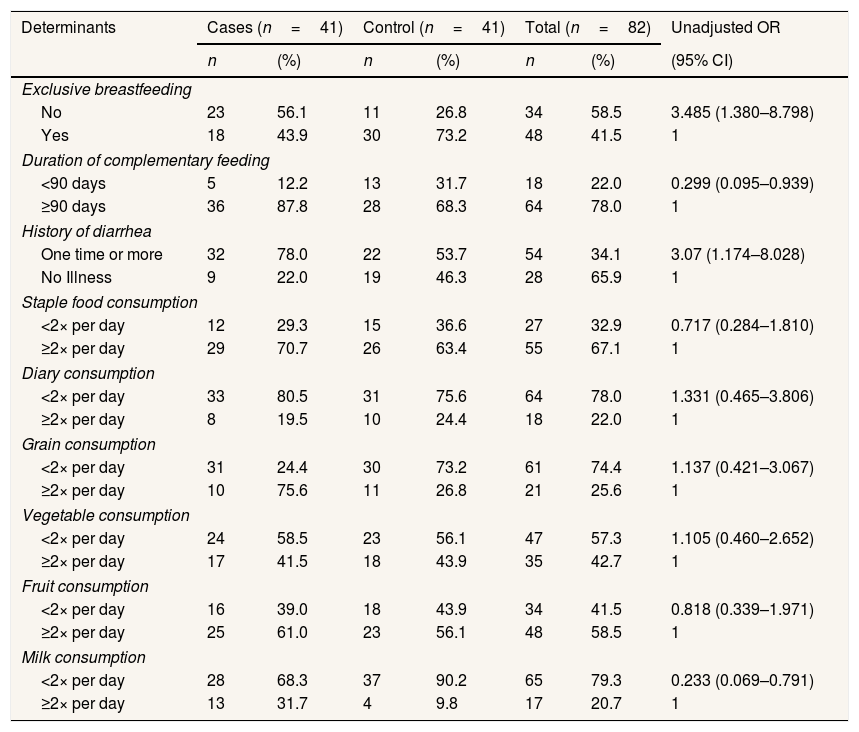
Bivariate analysis showed that no exclusive breastfeeding and having a history of diarrhea were risk factors of constant weight among children in Mangkutana. Duration of complementary feeding less than 90 days and milk consumption less than two times per day were found as a protective factor of constant weight (Table 2).
The determinant factor of constant weight among under two years old children.
| Determinants | Cases (n=41) | Control (n=41) | Total (n=82) | Unadjusted OR | |||
|---|---|---|---|---|---|---|---|
| n | (%) | n | (%) | n | (%) | (95% CI) | |
| Exclusive breastfeeding | |||||||
| No | 23 | 56.1 | 11 | 26.8 | 34 | 58.5 | 3.485 (1.380–8.798) |
| Yes | 18 | 43.9 | 30 | 73.2 | 48 | 41.5 | 1 |
| Duration of complementary feeding | |||||||
| <90 days | 5 | 12.2 | 13 | 31.7 | 18 | 22.0 | 0.299 (0.095–0.939) |
| ≥90 days | 36 | 87.8 | 28 | 68.3 | 64 | 78.0 | 1 |
| History of diarrhea | |||||||
| One time or more | 32 | 78.0 | 22 | 53.7 | 54 | 34.1 | 3.07 (1.174–8.028) |
| No Illness | 9 | 22.0 | 19 | 46.3 | 28 | 65.9 | 1 |
| Staple food consumption | |||||||
| <2× per day | 12 | 29.3 | 15 | 36.6 | 27 | 32.9 | 0.717 (0.284–1.810) |
| ≥2× per day | 29 | 70.7 | 26 | 63.4 | 55 | 67.1 | 1 |
| Diary consumption | |||||||
| <2× per day | 33 | 80.5 | 31 | 75.6 | 64 | 78.0 | 1.331 (0.465–3.806) |
| ≥2× per day | 8 | 19.5 | 10 | 24.4 | 18 | 22.0 | 1 |
| Grain consumption | |||||||
| <2× per day | 31 | 24.4 | 30 | 73.2 | 61 | 74.4 | 1.137 (0.421–3.067) |
| ≥2× per day | 10 | 75.6 | 11 | 26.8 | 21 | 25.6 | 1 |
| Vegetable consumption | |||||||
| <2× per day | 24 | 58.5 | 23 | 56.1 | 47 | 57.3 | 1.105 (0.460–2.652) |
| ≥2× per day | 17 | 41.5 | 18 | 43.9 | 35 | 42.7 | 1 |
| Fruit consumption | |||||||
| <2× per day | 16 | 39.0 | 18 | 43.9 | 34 | 41.5 | 0.818 (0.339–1.971) |
| ≥2× per day | 25 | 61.0 | 23 | 56.1 | 48 | 58.5 | 1 |
| Milk consumption | |||||||
| <2× per day | 28 | 68.3 | 37 | 90.2 | 65 | 79.3 | 0.233 (0.069–0.791) |
| ≥2× per day | 13 | 31.7 | 4 | 9.8 | 17 | 20.7 | 1 |
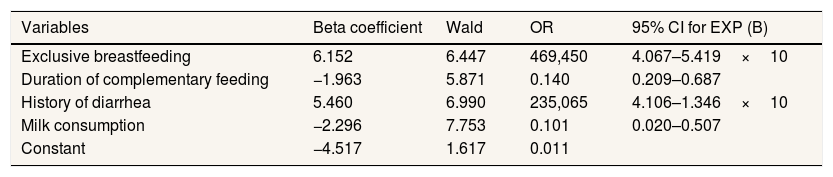
Table 3 presents the final explanatory model of constant weight based on multivariate analysis. It showed that Exclusive breastfeeding, the duration of complementary feeding, history of diarrhea, milk consumption patterns and interactions between exclusive breastfeeding and a history of infectious diseases have a relationship with constant body weight.
Factors associated with constant weight, multivariate analysis.
| Variables | Beta coefficient | Wald | OR | 95% CI for EXP (B) |
|---|---|---|---|---|
| Exclusive breastfeeding | 6.152 | 6.447 | 469,450 | 4.067–5.419×10 |
| Duration of complementary feeding | −1.963 | 5.871 | 0.140 | 0.209–0.687 |
| History of diarrhea | 5.460 | 6.990 | 235,065 | 4.106–1.346×10 |
| Milk consumption | −2.296 | 7.753 | 0.101 | 0.020–0.507 |
| Constant | −4.517 | 1.617 | 0.011 |
From the results of multivariate analysis, the form of multiple logistic regression models can be expressed in the mathematical equation as follows:
DiscussionIn the present study exclusive breastfeeding is associated with constant weight among children aged 12–24 months. Children who did not have exclusive breastfeeding have a risk of 3.485 experienced constant weight compared to children who have exclusive breastfeeding. These results in line with the previous study reported that breastfeeding was associated with weight gain.6,7
Exclusive breastfeeding is the provision of only breast milk without additional fluids or other foods until the babies reach 6 months old. The occurrence of malnutrition is closely related to milk production and the duration of breastfeeding. Weaning the baby too quickly will increase the likelihood of malnutrition. Children who are not offered exclusive breastfeeding up to 6 months of their birth have a risk suffer from a range of infectious diseases and undernutrition.2,8,9 Another study showed that the discontinuation of EBF before six months was associated with an increased incidence of diarrhea, fever, and ARIs. It was also associated with an increased incidence of wasting and underweight in childhood.10 This can be caused by excess immunology, nutrition, and nutrition from breastfeeding. An additional benefit of breastfeeding has a role in the prevention of malnutrition.
The Ministry of Health of the Republic of Indonesia is carrying out a complementary feeding program for all poor families with the target of providing complementary foods in the form of biscuits. The program is the provision of nutritional supplementation to complement nutritional needs to achieve bodyweight according to age. Every 100g of PMT contains 450 calories, 71g of carbohydrates, 14g of fat, and 9g of protein. PMT Toddler contains 10 vitamins (vitamins A, B1, B2, B3, B6, B12, D, E, K, and folic acid) and 7 minerals (iron, zinc, phosphorus, selenium, and calcium).11 The program is given within three months.
The current study showed that consumed complementary feeding minimum of three months and the frequency of milk consumption were significant as protective factors of constant weight was significant as protective factors of constant weight. This finding was supported by previous studies that infant feeding recommendations regarding portion sizes, meal frequency, nutrient-dense foods, and developing to eat support better growth during infancy and early childhood.6
In this study, around 65.9% of children had a history of diarrhea. Diarrheal disease with a higher probability of body constant. Childhood morbidity status, especially diarrhea, has been reported in other studies to harm the growth of children, specifically on weight gain. Diarrhea and other conditions that affect food intake and utilization, consequently affecting the nutritional status of children.12 Infection and malnutrition have always been intricately linked. The problem of immunodeficiency worldwide is mainly due to malnutrition. The relationship between malnutrition and diarrheal disease, like most infections, is two-way; that is, the nutritional state increase chance of the host response to infection, and infectious illness increase the chance of nutritional status.13
The model obtained from the multivariate analysis can estimate fixed body weight using exclusive breastfeeding variables, the duration of complementary breastfeeding from the Ministry of Health, history of infectious diseases, milk consumption patterns and interactions between exclusive breastfeeding and a history of infectious diseases This equation shows that the fixed body weight in children aged two years will add 6.152kg of body weight if given exclusive breastfeeding, the bodyweight remains in underweight will lose 1.963kg body weight if they consume complementary milk >90 days, the bodyweight remains in underweight will add 5.460kg of body weight if there is no history of infectious disease, the fixed weight of a two-year-old child will lose 2.29kg of body weight if they rarely consume milk, and the interaction between exclusive breastfeeding and a history of infectious disease will reduce 2.874kg weight who experience a fixed weight.
There is an interaction between exclusive breastfeeding and a history of diarrhea, which means that children who are not given exclusive breastfeeding are more at risk of experiencing a history of diarrhea and ultimately causing a fixed weight. Also, it can be seen that the most dominant factor affecting fixed body weight in this study is the exclusive breastfeeding variable.
The previous study also found that there was a significant difference in the incidence of infectious diseases in children under exclusive breastfeeding and non-exclusive breastfeeding.14 Another study states that babies who are not exclusively breastfed have a relationship with the incidence of ARI, where babies who are not exclusively breastfed have a 4.96 greater risk of experiencing an ARI than babies who are exclusively breastfed. The incidence of diarrheal disease also shows a significant difference in infants exclusively breastfed and infants who are given formula milk.15,16 Exclusive breast milk contains many antibodies specifically for the baby's immune system. Immunoglobulin A is a type of antibody substance that is well known in breast milk, it is tasked with making the inner lining of the intestinal mucosa to become a barrier to prevent pathological bacteria from entering.
ConclusionsExclusive breastfeeding during the first six months is crucial to support complementary feeding program in increasing the body weight status of children aged 12–24 months. Consumption of complementary feeding based on government direction is important in increasing the weight status of children aged 12–24 months.
Conflicts of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.