The 3rd International Nursing and Health Sciences Students and Health Care Professionals Conference (INHSP)
Más datosThis study aims to determine the correlation between Endothelin-1 levels and mean arterial pressure (MAP) with preeclampsia so that their combination can be used as the predictor of PE in early pregnancy.
MethodThis study used a cross-sectional study with a case-control design carried out in February to June 2020 in several hospitals and health centers in Makassar city, namely Dr. Wahidin Soedirohusodo General Hospital, Hasanuddin University State University Hospital, health center Bara Baraya, health center Mamajang, and health center Antang. Respondents in this study were divided into 37 pregnant women with preeclampsia and 53 pregnant women with normotension. This study's criteria for respondents were 20–35 years old, single pregnancy with > 20 weeks gestational. Data collected included education, body mass index (BMI), parity, the interval of pregnancy, and gestational age. ET-1 levels were determined using th ET-1 Elisa Kit with the ELISA method, and MAP was collected by measuring blood pressure when pregnant women came to health facilities.
ResultsThe mean serum ET-1 levels in the preeclampsia were highest than normotensive with a significant p-value of 0.001 (p<0.05). The MAP in the preeclampsia was highest than normotensive too, with a significant value of p-value 0.001 (p<0.05), and there is a positive correlation between ET-1 and MAP with r=0.34 and p-value 0.001 (p<0.05).
ConclusionThe combination of ET-1 and MAP can be considered as a prognostic factor to detect PE in early pregnancy.
Preeclampsia is a condition established in the presence of specific hypertension caused by pregnancy, increase in urine protein levels, and accompanied by disorders of the system of other organs at the age of pregnancy above 20 weeks. Diagnosis of hypertension in pregnancy can be enforced into preeclampsia if the new symptoms arise in the form of increased urine protein levels exceeding 300mg in 24h, the ratio of protein: serum urine ≥0.3 or protein gain as much as 30mg/dL (Dipping dip 1+).1
Preeclampsia is a condition that occurs only during pregnancy and is one of the three leading causes of maternal death in gestation, childbirth, and after childbirth and also the cause mortality and morbidity perinatal. Most babies born from preeclampsia mothers will experience stunted fetal growth, premature birth, and low birth weight, even to death. Children born from preeclampsia mothers will have a higher risk of metabolic diseases than children born from normal mothers.2,3
Many studies have reported that preeclampsia occurs due to a lousy presentation, so that the oxidative stress of the placenta causes endothelial cell damage. Increased Soluble Fms-like tyrosine kinase-1 (sFlt-1) resulted in decreased PIGF and VEGF, resulting in endothelial dysfunction, which led to an increase in the production of ET-1 and increased blood pressure. Many studies have also explained that endothelin-1 has a connection with the occurrence of preeclampsia due to its nature as a vasoconstrictor. According to these reports, ET-1 has been indicated to be associated with the pathogenesis of PE. Some cohort studies showed increased plasma levels of ET-1 in preeclampsia, with multiple studies indicating the circulation level of ET-1 correlates to the severity of the disease.4,5
MethodThis study used a cross-sectional study with a case–control design carried out from February to June 2020 and has received a recommendation of ethical approval with the protocol number UH19111014. This study was conducted in several hospitals and health centers in Makassar city, namely Dr. Wahidin Soedirohusodo General Hospital, Hasanuddin University State University Hospital, health center Bara Baraya, health center Mamajang, and health center Antang. Respondents in this study were divided into 37 pregnant women with preeclampsia and 53 pregnant women with normotension. Criteria for respondents in this study were a pregnant woman 20–35 years old, single pregnancies with >20 weeks gestational. Data collected included education, body mass index (BMI), parity, the distance of pregnancy, and the age of gestational. ET-1 Levels were determined using the ET-1 Elisa Kit with the ELISA method, and MAP was collected by measuring blood pressure when the pregnant women came to health facilities.
Data collection techniquesData related to demographics and obstetric history of the respondents were collected using a questionnaire through direct interviews with respondents. Meanwhile, researchers were assisted by laboratory personnel at the research hospital and health care for blood sampling. The collected samples are then centrifuged and stored in a refrigerator at −20°C. After all the samples had been collected, the serum ET-1 level was examined using the ET-1 Kit by the ELISA method at the Research Center Laboratory (HUM-RC) of Hasanuddin Medical University. The MAP was collected by measuring blood pressure when pregnant women came to health facilities.
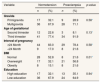
ResultSee Tables 1–3.
Demographic and obstetric characteristics of respondents.
| Variable | Normotension | Preeclampsia | p-value | ||
|---|---|---|---|---|---|
| n | (%) | n | (%) | ||
| Gravida | |||||
| Primigravida | 17 | 32.1 | 9 | 28.9 | 0.58* |
| Multigravida | 36 | 67.9 | 28 | 71.1 | |
| Age of gestational | |||||
| Second trimester | 12 | 22.6 | 3 | 8.1 | 0.13* |
| Third trimester | 41 | 77.4 | 34 | 91.9 | |
| Interval of pregnancy | |||||
| ≥24 Month | 44 | 83.0 | 29 | 78.4 | 0.58* |
| <24 Month | 9 | 17.0 | 8 | 21.6 | |
| BMI | |||||
| Normal | 28 | 52.8 | 8 | 21.6 | 0.01* |
| Overweight | 17 | 32.1 | 21 | 56.8 | |
| Obesity | 8 | 15.1 | 8 | 21.6 | |
| Education | |||||
| High education | 17 | 32.1 | 13 | 35.1 | 0.94* |
| Low education | 36 | 67.9 | 24 | 64.9 | |
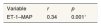
The correlation between ET-1 and MAP.
| Variable | r | p |
|---|---|---|
| ET-1–MAP | 0.34 | 0.001* |
Based on statistical tests in Table 1 showed the gravida, gestational age, pregnancy distance, income, and education did not differ significantly either in the normotensive and preeclampsia group (p>0.05). Meanwhile, the body mass index (BMI) showed a significant difference with a p-value of 0.01. Pregnancy women with high BMI are at 2× higher risk of preeclampsia than pregnant women with a normal BMI,6 and another study showed that the risk of PE increased from 4.3% in mothers with a BMI<20kg/m2 to 13.3% in mothers with a BMI>35kg/m2 [1]. Based on Table 2, it can be seen that there is a meaningful difference in ET-1 rate with a value of p=0.001, and there is also a meaningful MAP rate difference between the two groups with a value of p=0.001. These results are similar to some other research.7–9
The main findings in this study were that the correlation between ET-1 and MAP has a meaningful positive correlation (r=0.34 and p=0.001) (Table 3). That means the higher level of ET-1 results in a higher MAP value too. These results are similar to other studies.10,11
The failure of placentation and trophoblast invasion may interfere with the normal function of endothelial.12 The compounds derived by endothelial that may be played a role in the PE are Endothelin-1 (ET-1), an increase of ET-1 will also increase oxidative stress in the placenta. Endothelial cells play a role in cardiovascular settings by producing vasoactive agents, including vasodilator molecules and vasoconstrictor peptides. Increased smooth muscle sensitivity by ET-1 affects peripheral vascular and vascular hypertrophy and participates in regulating blood vessel muscle tonus.13 A vital stimulus to the release Et-1 is hypoxia, ischemic, and stress, which induces messenger transcription of RNA ET-1. In addition to the physical stimulation of endothelin production is also influenced by vasopressor hormones such as epinephrine, angiotensin II, and vasopressin arginine, transforming growth factor β (TGFβ), thrombin and Interleukin-1.14
ET-1 is a vasoconstrictor that can improve vascular resistance so that the diameter of blood vessels will be reduced and induced an increase of pressure on the blood vessels; in the end, there will be an increase in blood pressure or MAP. Endothelial cells have an essential role in producing and balancing vasoactive substances such as vasoconstrictor substances (ET-1 and Thromboxers) and Vasodilatators (NO and prostaglandins). Damaged the endothelial cells resulted in the imbalance of the levels of vasoactive substances in the blood. Increased smooth muscle sensitivity by ET-1 affects peripheral vascularity and vascular hypertrophy. An increase in the ET-1 concentration of PE is usually followed by a decline in prostacyclin and nitric oxide production. ET-1 plays a role in the pathogenesis of increased blood pressure.15 Endothelial cell damage that occurs due to high blood pressure induces an increase in plasma concentrations of ET-1 in hypertension pregnancy. An increase in the ET-1 production by small arterial endothelium can play a role not only in high blood pressure but also in accentuating the hypertrophic small artery remodeling in patients with moderate to severe hypertension.16
ConclusionThe serum ET-1 and MAP value levels can be used as a prognostic factor to detect PE in the early pregnancy, but still need another study to support examinations to be researched. Nevertheless, the term as supporting data can be an early marker of the pathophysiological risk factors for preeclampsia.
Conflicts of interestThe authors declare no conflict of interest.
Peer-review under responsibility of the scientific committee of the 3rd International Nursing, Health Science Students & Health Care Professionals Conference. Full-text and the content of it is under responsibility of authors of the article.