To establish the influence of clinical status at diagnosis and of gender on progression of HIV/AIDS determined by clinical-biological factors in patients from Cordoba City (Argentina) from 1995 to 2005).
MethodsGender and clinical and laboratory data were evaluated by descriptive statistics, non-parametric survival analysis, and generalized linear models at the beginning of the study (diagnosis) and at the end (hospital records, n=209).
ResultsAt diagnosis, women (n=28, 13.4%) had a higher probability of being asymptomatic than men (n=181, 86.6%). High viremia was associated with advanced clinical stages, but was inversely related to CD4 count. Truncated Kaplan-Meier curves were similar for both sexes. The probability of not having AIDS criteria at the end of the study was higher in patients without these criteria at diagnosis. Women had a higher probability of having AIDS at the end of the follow-up than men. In contrast, men had a higher prevalence of venereal diseases (n=38, 21%), dysmetabolic profile (n=14, 7.7%) and positive serology for opportunists (n=31, 17.1%). Marker diseases were mainly represented by internal mycosis and waste syndrome, although less specific findings (anemia, oral lesions) were also associated with progression.
ConclusionsUsing an integrative approach, high viremia was critically linked to clinical and lymphocyte impairment. Early diagnosis was a major determinant of clinical course, with women having a worse prognosis. However, men were diagnosed in clinically advanced stages and with other non-HIV-related entities, which could affect progression. These findings should be integrated into the planning of preventive strategies.
Establecer la influencia de la condición médica al diagnóstico y del sexo en la evolución del VIH/Sida determinada por factores clínico-biológicos en pacientes de la ciudad de Córdoba (Argentina, 1995–2005).
MétodosEl sexo, los datos clínicos y los de laboratorio fueron evaluados por estadística descriptiva, análisis de supervivencia no paramétrico y modelos lineales generalizados al inicio (diagnóstico) y al final del estudio (registro hospitalario, 209 casos).
ResultadosLas mujeres (n=28, 13,4%) tienen mayor probabilidad de estar asintomáticas que los hombres (n=181, 86,6%) en el momento del diagnóstico. La viremia alta está asociada con estadios clínicos avanzados, pero está inversamente relacionada con el de CD4. Las curvas truncadas de Kaplan-Meier son similares para ambos sexos. La probabilidad de no tener criterios de sida al final del estudio está incrementada para los pacientes diagnosticados sin ellos. Además, las mujeres tienen mayor probabilidad de presentar sida que los hombres al finalizar el seguimiento recuento. No obstante, ellos mostraron una elevada prevalencia de enfermedades venéreas (n=38, 21%), perfil dismetabólico (n=14, 7,7%) y serología para oportunistas (n=31, 17,1%). Las enfermedades marcadoras fueron principalmente micosis internas y síndrome consuntivo, aunque hallazgos menos específicos (anemia, lesiones orales) también se asociaban a la progresión.
ConclusionesUtilizando un enfoque integrador, la viremia estuvo muy ligada al empeoramiento clínico y linfocitario, siendo el diagnóstico temprano un determinante mayor de evolución, con las mujeres teniendo peor pronóstico. Sin embargo, los hombres fueron diagnosticados avanzados clínicamente, con otros problemas no asociados al VIH que podrían afectar su evolución. Estos resultados deberían ser integrados en el planeamiento sanitario de prevención.
The illness caused by the human immunodeficiency virus (HIV) has a chronic progression. It starts with an acute syndrome and serological conversion, and is then followed by a long-term phase of clinical latency. Ultimately, AIDS-related complex and acquired immunodeficiency syndrome (AIDS) constitute the final stage. The virus replicates continuously into CD4-positive lymphocytes, thereby causing their depletion. Since these cells are a critical point for adaptive immunity, the infection predisposes to opportunistic infections and malignancies (opportunists/opportunism: diseases which appear only with immunocompromise).1
UNAIDS has estimated that at least 40 million people live with HIV/AIDS, with 3 million deaths and 5 million new cases every year. The number of HIV/AIDS cases notified in Argentina since 2001, when the obligatory notification began, was 34,803 with a male prevalence. The majority of people living with this infection reside in Capital Federal (30%), Buenos Aires (30%), Cordoba (6%) and Santa Fe (4%). In the year 2005, Argentina exhibited rates of 12.9 HIV cases and of 4.3 AIDS cases per 100,000 persons, which have tended to decrease since the year 1997, when HAART was introduced. Regarding Cordoba, the rate of HIV cases per 100,000 persons was 11.6 in 2005. The most relevant transmission way was sexual (82% of women and 73% of men, of which 31% corresponded to homosexual practice). Also, 4.6% of women and 14.5% of men used injected drugs. The 4.3% of the cases were due to vertical transmission.2
The epidemiological characterization of the infection is difficult due to its varying spread patterns in different regions worldwide.3 Consequently, infection behaviour should be analyzed thoroughly in each population in the context of the general pandemic reality.4 Furthermore, the integration of different statistical methods is necessary, so that reliable tools may be obtained for medical decision mechanisms. Patient surveys should be realized by medical institutions in order to improve engagement and retention in care, and to achieve an organizational self-assessment to effect operational changes that minimize barriers to care.5 Subsequently, this study uses an integral trend of HIV/AIDS in an Argentinean city, and its purpose is to establish the role of the diagnostic condition and the gender influence in this infection by establishing the close relationship between medical status at diagnosis and during evolution, by means of analysis of the clinical and biological markers of the HIV infection.
MethodsSubjects and settingData were collected from hospital records (Hospital Nacional de Clínicas, Universidad Nacional de Córdoba) anonymously in agreement with ethical concerns for 209 adult patients from the Cordoba City (Argentina) in the period 1995–2005. Non experimental procedures were performed for this prospecting work made in retrospect, with a sample under current medical control being described.
Patients were classified according to the Control Disease Center criteria, regarding the peripheral blood CD4 count (1: >500, 2: 200–499, 3: <200CD4cells/μl), plasmatic viral load (< or >100 000copies/mL-VL-) and clinical categories (A: health or non-related diseases; B: related diseases; C: marker diseases, opportunism).6 Asymptomatic people were tested in regard to antecedents of risk behaviours. Patients who exhibited <200-CD4, >105-VL and/or opportunistic pathologies were obligatorily treated with antiretroviral drugs. Individuals who presented AIDS criteria (clinical category C and/or level 3 of CD4) at the diagnostic instance were considered lately-diagnosed patients. The transmission ways were in accordance with governmental data.2
LaboratoryCD4 and VL were assayed by flow cytometry and RT-PCR, respectively.7,8 Other biochemical probes had been performed using standard commercial kits, provided by Wiener Lab (Argentina).
Statistical analysisResults are expressed as mean (SD). Clinical-biological records were studied during diagnosis and progression, with the descriptive analyses examining the prevalence of clinical and biochemical parameters. Data recorded at the time of serological confirmation were analyzed by two different approaches. First, the clinical stage was considered as the response variable, and a proportional odds model was fitted,9 with gender and VL factors as covariates in the linear predictor. Then, the association between CD4, gender and VL was assessed using a log-linear model for ordinal data.10 In the construction of the interaction terms, this association model considers scores for the three ordered CD4 categories.
The incidence rate of opportunism was calculated for each gender, assuming that individual times could vary (IR=new cases of opportunism/Σ individual times free of opportunism).11 Also, using the appearance of marker diseases (opportunism) as the clinical evolution indicator, the cumulative probability was estimated for time free of these by the Kaplan-Meier method,12 with gender differences being investigated by the log-rank test.13
Finally, the association between the initial and final medical status, i.e. at the diagnosis and at the end of the study, was analyzed by log-linear models,10 with patients being classified according to sex and presence/absence of AIDS criteria, at each instance. This categorization of initial and final stages avoids treatment being a confounding factor, since treatment was strictly given to every patient diagnosed with AIDS. Newly diagnosed patients (<1 evolution year) were excluded, since they did not have enough time to change the category.
The significance level used was α=0.05. Data were analyzed using InfoStat2007e.1 (InfoStat Group, http://www.infostat.com.ar) and R version 2.0.1 (R Development Core Team, http://www.R-project.org).
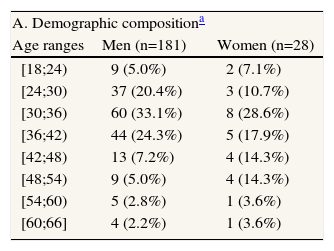
Results181 men (86.6%) were of mean age 35.2±8.7 (range=18–66), and 28 women (13.4%) were 38.1±10.4 (range=20–61). This included 15% men and 25% women who had been recently diagnosed (<1 year from the diagnosis). Patients were enrolled at 27.11±1.84 (men) and 4.78±2.34 (women) individuals per year, involving mainly the 24–42 year-old range at different clinical stages (table 1).
Clinical-epidemiological profile of the studied sample
| A. Demographic compositiona | ||
| Age ranges | Men (n=181) | Women (n=28) |
| [18;24) | 9 (5.0%) | 2 (7.1%) |
| [24;30) | 37 (20.4%) | 3 (10.7%) |
| [30;36) | 60 (33.1%) | 8 (28.6%) |
| [36;42) | 44 (24.3%) | 5 (17.9%) |
| [42;48) | 13 (7.2%) | 4 (14.3%) |
| [48;54) | 9 (5.0%) | 4 (14.3%) |
| [54;60) | 5 (2.8%) | 1 (3.6%) |
| [60;66] | 4 (2.2%) | 1 (3.6%) |
| B. Diagnostic medical status according to the viral load (copies/ml) | ||||
| CDC stagesb | Men (n=181) | Women (n=28) | ||
| <105 (n=136) | >105 (n=45) | <105 (n=18) | >105 (n=10) | |
| A1 | 72 (53.0%) | 9 (20.0%) | 6 (33.3%) | 2 (20.0%) |
| A2 | 40 (29.4%) | 6 (13.3%) | 10 (55.6%) | 2 (20.0%) |
| A3 | 2 (1.5%) | 1 (2.2%) | 2 (11.1%) | 2 (20.0%) |
| B1 | 10 (7.4%) | 2 (4.5%) | 0 (0.0%) | 0 (0.0%) |
| B2 | 3 (2.2%) | 4 (8.9%) | 0 (0.0%) | 1 (10.0%) |
| B3 | 1 (0.7%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| C1 | 1 (0.7%) | 1 (2.2%) | 0 (0.0%) | 0 (0.0%) |
| C2 | 1 (0.7%) | 2 (4.5%) | 0 (0.0%) | 2 (20.0%) |
| C3 | 6 (4.4%) | 20 (44.4%) | 0 (0.0%) | 1 (10.0%) |
71.8% men presented stage A. Nonetheless, 37.6% had other negative medical conditions (not specifically related to AIDS), including abnormal laboratory tests. These laboratory findings were: sustained high IgG in mononucleosis-like syndromes (Toxoplasma spp., cytomegalovirus, Epstein-Barr virus) (n=31), dyslipemia (n=14), altered asymptomatic hepatogram (n=8), sustained high IgG for other pathogens (Trypanosoma cruzi, hepatitis B and A viruses) (n=4), among others (n=5). Other sexually transmitted diseases were present in 21% of patients (early syphilis: 18, chronic hepatitis: 13, papilloma virus: 5, genital herpes simplex: 2, molluscum contagiosum: 1). There were 7 cases of acute retroviral syndrome, with stage B being principally represented by polymyositis, oral candidiasis, herpes zoster, leucopoenia and thrombocytopenia. Anaemia was also a common finding in progressing patients (n=2, B1; n=1, C2; n=10, C3). Oral lesions were found in 16 persons, 13 with AIDS, corresponding to oropharynx candidiasis and oral hairy leukoplakia. When CD4 decreased, seborrheic dermatitis, acute respiratory infections, Kaposi’s sarcoma and waste syndrome emerged. Pulmonary pneumocystosis (n=11), oesophagic candidiasis (n=4), disseminated histoplasmosis (n=2), progressive multifocal leukoencephalopathy (n=2) and retinitis by cytomegalovirus (n=1) conformed the marker illnesses. Other advanced clinical events were chronic diarrhoea, fever of an unknown origin, severe thrombocytopenia, peripheral neuropathy and persistent generalized pruritus, all without a clear etiological diagnosis. Pulmonary tuberculosis complicated with meningitis was also found.
85.7% women were diagnosed as being asymptomatic, with 14.3% being detected during routine serological control in obstetric patients. Also, oropharynx candidiasis was identified in a B2 case. The rest were considered as AIDS cases, presenting consumption with anaemia and oral hairy leukoplakia, herpes zoster, pulmonary pneumocystosis, cerebral toxoplasmosis, meningoencephalitis by Cryptococcus, persistent polyadenopathy and neutropenia.
The proportional odds model (deviance=4.958, df=4, p=0.292) showed that women have higher odds (4.13 times) of presenting a better clinical condition than men (p=0.023), for a fixed VL. The odds of having an advanced clinical stage are higher (12.41 times) for VL >100,000copies/mL (p<0.001) for a given gender. Furthermore, the association log-linear model was suitable for CD4 (deviance=8.71, df=5, p=0.121) showing that the CD4 is inversely related to VL (p<0.001), but is not associated to gender (p=0.099).
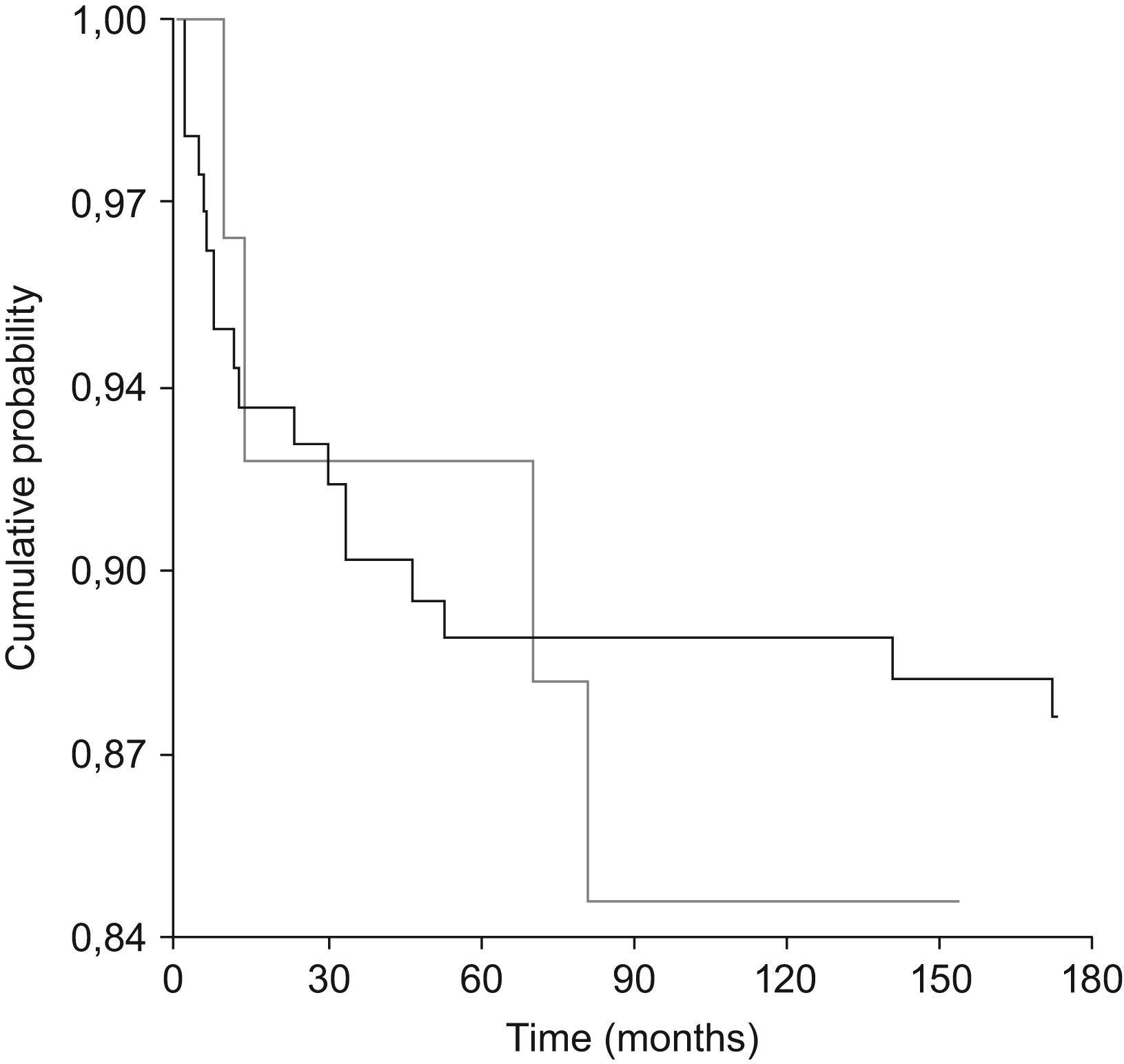
EvolutionThe mean follow-up time was around four years (range: <1–10 years). For both genders, 10 opportunistic cases occurred per 100 person-years of follow-up, with about 1.6 episodes per person taking place during their evolution. The curves of Kaplan-Meier, depicted in figure.1, did not show any differences between genders (X2=0.163, df=1, p=0.686). Data from 31 men and 2 women (17% vs. 7%) were considered as truncated, since they were diagnosed already ill.
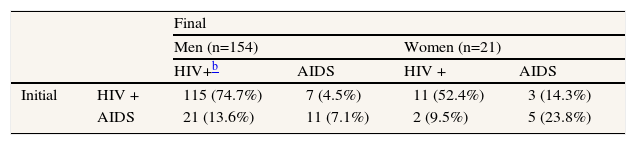
Regarding medical re-stratification (deviance=0.005, df=2, p=1) described in the Table 2, the odds of not having AIDS criteria when the follow-up finishes are higher for patients (8.76 times) being diagnosed without AIDS (p<0.001), for a given gender. Also, women have higher odds (4.65 times) of presenting AIDS at the end of the study than men (p=0.003), given an initial condition.
DiscussionThe HIV/AIDS management involves early detection and close evolutive monitoring, with epidemiological studies in developing countries being imperative to support sanitary strategies.14 In the present work, although many patients were at stage A, a several advanced cases were still found. Moreover, the deleterious effect of VL on CD4 and the clinical condition could be seen from the point of diagnosis. Despite the fact that gender did not affect the CD4, men had a greater possibility than women of being clinically impaired at the time of diagnosis. Consequently, early detection should be strongly encouraged to improve prognosis and infection control,15 especially in male individuals, considering that prevention messages are not being performed appropriately.16 Among initial findings, the common occurrence of venereal diseases in the males accounted for both behavioural and pathological indicators, which could be preliminary motives for consulting.17 The clinical and laboratory prevalence for opportunistic infections and/or debilitating conditions justified that their screening included the asymptomatic patients. Chagas disease deserves special attention, although it is not distributed worldwide, but it depends on the immune status,18 with geographic variations of tropical endemic infections being often not considered.19 During successive medical appointments, hemogram alterations were commonly found, especially anaemia, whose frequency increased as infection progressed. Oral lesions exhibited the same behaviour with regard to progression, as also did seborrhoea, respiratory infections and Kaposi sarcoma, with these being related to decreasing levels of CD4. Due to the relevance of oral lesions, often sub-diagnosed and/or inadequately treated, buccal evaluation is encouraged.20 Another problem linked to low CD4 was the waste syndrome (principal marker disease together with pneumocystosis), followed by other disseminated mycosis and neurological affections. Nonetheless, it is necessary to bear in mind that opportunistic diseases are not reciprocally excluding, and that other problems with an unclear etiopathology can also appear.
Different statistical models were applied, since the incidence measures only give summary information. The Kaplan-Meier method allowed evolution to be studied, by taking marker diseases as the progression criteria, although no differences between genders were found. However, initially ill people were not considered, thus causing a different data truncation for each one. Indeed, the initial clinical status is relevant for gender comparisons and infection management.21 For categorical data, generalized linear models give a complete description about associations, with increased power for detecting them.22
In the analysis of medical re-stratification, it was confirmed that an early diagnosis was important in patient prognosis, since individuals without initial AIDS criteria tended to stay in this situation at the end of the study. Regarding gender, under the mentioned methodological conditions (analyzing the HIV/AIDS evolution in an alive population under sanitary control), female evolution exhibits a worse prognosis than men, which will imply further studies in order to develop complementary medical actions to modulate their pathological progression. There is ongoing debate concerning a potential gender effect. Several factors may be involved in this response, although a previous work established that no differences between sexes existed respect to antiretroviral therapy.23 In the same research, low patient adherence and presence of pharmacological toxicity (evaluated in a specific subgroup under treatment) were the main determinants of therapeutic failure. However, in another work, women benefited less from care, even though they were admitted at earlier stages and offered standardized therapies with unclear reasons, requiring further studies.24 In addition, the CD4 predicting value for specific sociodemographic groups is discussed,25 with VL having higher prognostic strength.26
Concerning the promotion of norms regarding risk reduction, the peer education and gender-specific HIV prevention interventions may be useful.27 In this sense, interventions seeking to promote gender equity and to reduce HIV/STI may be more effective when the socioeconomic context of gender ideologies is assessed and addressed.28 HIV prevention programs should be designed to increase knowledge about HIV transmission, treatment, prevention and personal risk of contraction as well as correct misconceptions about individuals with HIV or AIDS and promote sex communication among partners. Since gender-related behaviours have been proposed as risk determinants, the measures of relational attitudes and experiences become relevant to characterize sexual risk, especially among men.29
The proper evaluation of HIV urban behaviour should be focused for different populations, since it allows developing accurate health policies. Also, the integration of analytical tests may enhance the outcomes’ value. Overall, an integrative assessment, which studies of clinical-biological factors by different methodologies, allows the close relationship between diagnostic stages and progression to be accomplished, in the polymorphic long-term HIV infection.